User:Mr. Ibrahem/Urinary tract infection
Template:Good article is only for Wikipedia:Good articles.
| Urinary tract infection | |
|---|---|
| Other names | Acute cystitis, simple cystitis, bladder infection, symptomatic bacteriuria |
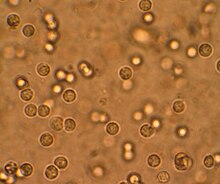 | |
| Multiple white cells seen in the urine of a person with a urinary tract infection using microscopy | |
| Specialty | Infectious disease |
| Symptoms | Pain with urination, frequent urination, feeling the need to urinate despite having an empty bladder[1] |
| Causes | Most often Escherichia coli[2] |
| Risk factors | Female anatomy, sexual intercourse, diabetes, obesity, family history[2] |
| Diagnostic method | Based on symptoms, urine culture[3][4] |
| Differential diagnosis | Vulvovaginitis, urethritis, pelvic inflammatory disease, interstitial cystitis[5] |
| Treatment | Antibiotics (nitrofurantoin or trimethoprim/sulfamethoxazole)[6] |
| Frequency | 152 million (2015)[7] |
| Deaths | 196,500 (2015)[8] |
A urinary tract infection (UTI) is an infection that affects part of the urinary tract.[1] When it affects the lower urinary tract it is known as a bladder infection (cystitis) and when it affects the upper urinary tract it is known as a kidney infection (pyelonephritis).[9] Symptoms from a lower urinary tract infection include pain with urination, frequent urination, and feeling the need to urinate despite having an empty bladder.[1] Symptoms of a kidney infection include fever and flank pain usually in addition to the symptoms of a lower UTI.[9] Rarely the urine may appear bloody.[6] In the very old and the very young, symptoms may be vague or non-specific.[1][10]
The most common cause of infection is Escherichia coli, though other bacteria or fungi may sometimes be the cause.[2] Risk factors include female anatomy, sexual intercourse, diabetes, obesity, and family history.[2] Although sexual intercourse is a risk factor, UTIs are not classified as sexually transmitted infections (STIs).[11] Kidney infection, if it occurs, usually follows a bladder infection but may also result from a blood-borne infection.[12] Diagnosis in young healthy women can be based on symptoms alone.[4][13] In those with vague symptoms, diagnosis can be difficult because bacteria may be present without there being an infection.[14] In complicated cases or if treatment fails, a urine culture may be useful.[3]
In uncomplicated cases, treatment is with a short course of antibiotics such as nitrofurantoin, fosfomycin, or trimethoprim/sulfamethoxazole.[6][13] Resistance to many of the antibiotics used to treat this condition is increasing.[1] In complicated cases, a longer course or intravenous antibiotics may be needed.[6] If symptoms do not improve in two or three days, further diagnostic testing may be needed.[3] Phenazopyridine may help with symptoms.[1] In those who have bacteria or white blood cells in their urine but have no symptoms, antibiotics are generally not needed,[15] although during pregnancy is an exception.[16] In those with frequent infections, a short course of antibiotics may be taken as soon as symptoms begin or long-term antibiotics may be used as a preventive measure.[17]
About 150 million people develop a urinary tract infection in a given year.[2] They are more common in women than men.[6] In women, they are the most common form of bacterial infection.[18] Up to 10% of women have a urinary tract infection in a given year, and half of women have at least one infection at some point in their lifetime.[4][6] They occur most frequently between the ages of 16 and 35 years.[6] Recurrences are common.[6] Urinary tract infections have been described since ancient times with the first documented description in the Ebers Papyrus dated to c. 1550 BC.[19]
References[edit]
- ^ a b c d e f "Urinary Tract Infection". Centers for Disease Control and Prevention (CDC). 17 April 2015. Archived from the original on 22 February 2016. Retrieved 9 February 2016.
- ^ a b c d e Flores-Mireles, AL; Walker, JN; Caparon, M; Hultgren, SJ (May 2015). "Urinary tract infections: epidemiology, mechanisms of infection and treatment options". Nature Reviews. Microbiology. 13 (5): 269–84. doi:10.1038/nrmicro3432. PMC 4457377. PMID 25853778.
- ^ a b c Colgan R, Williams M, Johnson JR (2011-09-01). "Diagnosis and treatment of acute pyelonephritis in women". American Family Physician. 84 (5): 519–26. PMID 21888302.
- ^ a b c Nicolle LE (2008). "Uncomplicated urinary tract infection in adults including uncomplicated pyelonephritis". Urol Clin North Am. 35 (1): 1–12, v. doi:10.1016/j.ucl.2007.09.004. PMID 18061019.
- ^ Caterino, Jeffrey M.; Kahan, Scott (2003). In a Page: Emergency medicine. Lippincott Williams & Wilkins. p. 95. ISBN 9781405103572. Archived from the original on 2017-04-24.
- ^ a b c d e f g h Salvatore S, Salvatore S, Cattoni E, Siesto G, Serati M, Sorice P, Torella M (June 2011). "Urinary tract infections in women". European Journal of Obstetrics, Gynecology, and Reproductive Biology. 156 (2): 131–6. doi:10.1016/j.ejogrb.2011.01.028. PMID 21349630.
- ^ GBD 2015 Disease and Injury Incidence and Prevalence, Collaborators. (8 October 2016). "Global, regional, and national incidence, prevalence, and years lived with disability for 310 diseases and injuries, 1990–2015: a systematic analysis for the Global Burden of Disease Study 2015". Lancet. 388 (10053): 1545–1602. doi:10.1016/S0140-6736(16)31678-6. PMC 5055577. PMID 27733282.
{{cite journal}}:|first1=has generic name (help)CS1 maint: numeric names: authors list (link) - ^ GBD 2015 Mortality and Causes of Death, Collaborators. (8 October 2016). "Global, regional, and national life expectancy, all-cause mortality, and cause-specific mortality for 249 causes of death, 1980–2015: a systematic analysis for the Global Burden of Disease Study 2015". Lancet. 388 (10053): 1459–1544. doi:10.1016/S0140-6736(16)31012-1. PMC 5388903. PMID 27733281.
{{cite journal}}:|first1=has generic name (help)CS1 maint: numeric names: authors list (link) - ^ a b Lane, DR; Takhar, SS (August 2011). "Diagnosis and management of urinary tract infection and pyelonephritis". Emergency Medicine Clinics of North America. 29 (3): 539–52. doi:10.1016/j.emc.2011.04.001. PMID 21782073.
- ^ Woodford, HJ; George, J (February 2011). "Diagnosis and management of urinary infections in older people". Clinical Medicine. 11 (1): 80–3. doi:10.7861/clinmedicine.11-1-80. PMC 5873814. PMID 21404794.
- ^ Study Guide for Pathophysiology (5 ed.). Elsevier Health Sciences. 2013. p. 272. ISBN 9780323293181. Archived from the original on 2016-02-16.
- ^ Introduction to Medical-Surgical Nursing. Elsevier Health Sciences. 2015. p. 909. ISBN 9781455776412. Archived from the original on 21 March 2020. Retrieved 17 September 2017.
- ^ a b "Therapeutics Initiative | [135] Empiric Antibiotic Therapy for Uncomplicated Lower Urinary Tract Infections". Therapeutics Initiative. Archived from the original on 17 April 2022. Retrieved 25 September 2022.
- ^ Jarvis, William R. (2007). Bennett & Brachman's hospital infections (5th ed.). Philadelphia: Wolters Kluwer Health/Lippincott Williams & Wilkins. p. 474. ISBN 9780781763837. Archived from the original on 2016-02-16.
- ^ Ferroni, M; Taylor, AK (November 2015). "Asymptomatic Bacteriuria in Noncatheterized Adults". The Urologic Clinics of North America. 42 (4): 537–45. doi:10.1016/j.ucl.2015.07.003. PMID 26475950.
- ^ Glaser, AP; Schaeffer, AJ (November 2015). "Urinary Tract Infection and Bacteriuria in Pregnancy". The Urologic Clinics of North America. 42 (4): 547–60. doi:10.1016/j.ucl.2015.05.004. PMID 26475951.
- ^ "Recurrent uncomplicated cystitis in women: allowing patients to self-initiate antibiotic therapy". Rev Prescire. 23 (146): 47–9. November 2013. PMID 24669389.
- ^ Colgan, R; Williams, M (2011-10-01). "Diagnosis and treatment of acute uncomplicated cystitis". American Family Physician. 84 (7): 771–6. PMID 22010614.
- ^ Al-Achi, Antoine (2008). An introduction to botanical medicines : history, science, uses, and dangers. Westport, Conn.: Praeger Publishers. p. 126. ISBN 978-0-313-35009-2. Archived from the original on 2016-05-28.
