User:Mr. Ibrahem/Diabetic neuropathy
| Mr. Ibrahem/Diabetic neuropathy | |
|---|---|
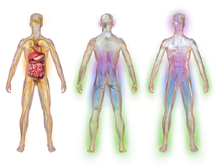 | |
| Areas affected by diabetic neuropathy | |
| Specialty | Neurology |
| Symptoms | Peripheral: Numbness, tingling, or weakness of the limbs[1] Autonomic: Urinary incontinence, gastroparesis, sexual dysfunction[2] Focal: Carpel tunnel, cranial neuropathy[3] |
| Complications | Diabetic foot[4] |
| Types | Peripheral, autonomic, focal, poximal[5] |
| Causes | Diabetes[5] |
| Risk factors | Poorly controlled diabetes, being overweight, high blood pressure, high cholesterol, kidney disease, alcohol, smoking[4] |
| Diagnostic method | Examination, electrophysiology testing[6] |
| Treatment | Diabetes and blood pressure control[4] |
| Medication | Gabapentin, pregabalin, duloxetine, venlafaxine, topical salicylates[7] |
| Frequency | Common[4][6] |
Diabetic neuropathy is nerve damage due to diabetes.[5] Symptoms depend on the location of damage: with peripheral neuropathy resulting in numbness, tingling, or weakness of the limbs;[1] autonomic neuropathy resulting in urinary incontinence, gastroparesis, or sexual dysfunction;[2] focal neuropathy such as carpel tunnel or cranial neuropathy;[3] or poximal neuropathy with hip or thigh pain.[8] Complications can include a diabetic foot and neuropathic arthropathy.[4][6]
It can occur as a result of any type of diabetes.[6] Risk factors include poorly controlled diabetes, being overweight, high blood pressure, high cholesterol, kidney disease, alcohol, and smoking.[4] The underlying mechanism involves direct damage to nerves and the small blood vessels that supply them from high blood sugar.[4][6] Diagnosis may be by examination or electrophysiology testing.[6]
Treatment may include gabapentin, pregabalin, duloxetine, venlafaxine, or topical salicylates.[7] Opioids and tricyclic antidepressants are generally not recommended.[7] Other measures include properly managing diabetes, blood pressure, and cholesterol.[4]
Up to half of people with diabetes have peripheral neuropathy, more than 30% have autonomic neuropathy, and less than 10% have carpal tunnel.[4] The peripheral form of the disease was first clearly described in 1864 by Marchall de Calvi while the autonomic form was first described in the 1900s.[6]
References[edit]
- ^ a b "Peripheral Neuropathy | NIDDK". National Institute of Diabetes and Digestive and Kidney Diseases. Archived from the original on 28 May 2021. Retrieved 3 August 2021.
- ^ a b "Autonomic Neuropathy | NIDDK". National Institute of Diabetes and Digestive and Kidney Diseases. Archived from the original on 17 April 2021. Retrieved 3 August 2021.
- ^ a b "Focal Neuropathies | NIDDK". National Institute of Diabetes and Digestive and Kidney Diseases. Archived from the original on 28 May 2021. Retrieved 3 August 2021.
- ^ a b c d e f g h i "What Is Diabetic Neuropathy? | NIDDK". National Institute of Diabetes and Digestive and Kidney Diseases. Archived from the original on 30 July 2021. Retrieved 3 August 2021.
- ^ a b c "Diabetic Neuropathy | NIDDK". National Institute of Diabetes and Digestive and Kidney Diseases. Archived from the original on 19 May 2021. Retrieved 3 August 2021.
- ^ a b c d e f g Jameson, J. Larry; Groot, Leslie J. De (18 May 2010). Endocrinology - E-Book: Adult and Pediatric. Elsevier Health Sciences. p. 985. ISBN 978-1-4557-1126-0. Archived from the original on 28 August 2021. Retrieved 3 August 2021.
- ^ a b c Falk, J; Thomas, B; Kirkwood, J; Korownyk, CS; Lindblad, AJ; Ton, J; Moe, S; Allan, GM; McCormack, J; Garrison, S; Dugré, N; Chan, K; Kolber, MR; Train, A; Froentjes, L; Sept, L; Wollin, M; Craig, R; Perry, D (May 2021). "PEER systematic review of randomized controlled trials: Management of chronic neuropathic pain in primary care". Canadian family physician Medecin de famille canadien. 67 (5): e130–e140. doi:10.46747/cfp.6705e130. PMID 33980642.
- ^ "Proximal Neuropathy | NIDDK". National Institute of Diabetes and Digestive and Kidney Diseases. Archived from the original on 18 April 2021. Retrieved 3 August 2021.
