User:DerekvG/sandbox/pg braintumor pt1
| DerekvG/sandbox/pg braintumor pt1 |
|---|
A brain tumor is an intracranial solid neoplasm, a tumor (defined as an abnormal growth of cells) within the brain or the central spinal canal.
Brain tumors include all tumors inside the cranium or in the central spinal canal. They are created by an abnormal and uncontrolled cell division, normally either in the brain itself (neurons, glial cells (astrocytes, oligodendrocytes, ependymal cells, myelin-producing Schwann cells), lymphatic tissue, blood vessels), in the cranial nerves, in the brain envelopes (meninges), skull, pituitary and pineal gland, or spread from cancers primarily located in other organs (metastatic tumors).
Any brain tumor is inherently serious and life-threatening because of its invasive and infiltrative character in the limited space of the intracranial cavity. However, brain tumors (even malignant ones) do not automatically cause death. Brain tumors or intracranial neoplasms can be cancerous (malignant) or non-cancerous (benign); however, the definitions of malignant or benign neoplasms differs from those commonly used in other types of cancerous or non-cancerous neoplasms in the body. Its threat level depends on the combination of factors like the type of tumor, its location, its size and its state of development. Because the brain is well protected by the skull, the early detection of a brain tumor only occurs when diagnostic tools are directed at the intracranial cavity. Usually detection occurs in advanced stages when the presence of the tumor has side effects that cause unexplained symptoms.
Primary (true) brain tumors are commonly located in the posterior cranial fossa in children and in the anterior two-thirds of the cerebral hemispheres in adults, although they can affect any part of the brain.
Taxonomy of brain tumors[edit]
By location and origin of the neoplasm[edit]
Primary brain tumors[edit]
Primary neoplasms of the brain are tumors that originate in the intracranial sphere or the central spinal canal, based on the organic tissus that make up the brain and the spinal cord. From the brain-lemma we can learn a lot of things about the composition of the brain from different types of organic tissues. For the purpose of this article we will discuss only some types.
- The brain itself is composed of neurons and glia (that function primarily as the physical support for neurons). The neurontissue itself is rarely the basis for a tumor, tumors of the glailcells are glioma and often are of the cancerous type.
- The brain is surrounded by a system of connective tissue membranes called meninges that separate the skull from the brain. Tumors of the meninges are meningioma and are often benign neoplasms.
- Below the brain is pituitary and pineal gland which could be the basis for its own -albeit rare- kind of benign glandular neoplasms.
Secondary braintumors[edit]
Secondary tumors of the brain are metastatic tumors that invaded the intracranial sphere from cancers primarily located in other organs. This means that a (malignant) cancerous neoplasm has developed in another organ elsewhere in the body and that cancer cells leak from that primary tumor. The leaked cells enter the lymphatic system and blood vessels, circulate through the bloodstream, and are deposited (strand in the small blood vessels in the brain) within normal tissue elsewhere in the body, in this case in the brain. There these cells continue growing & dividing and become another invasive neoplasm of the primary cancers tissue. Secondary tumors of the brain are very common in the terminal phases of patients with an incurable metastased cancer , most common types of cancers that bring about secondary tumors of the brain are lung cancer, breast cancer and malignant melanoma (skin cancer), kidney cancer and cancer of the colon (in decreasing order of frequency).
Unfortunately enough this is the most common cause of neoplasms in the intracranial cavity.
The skull bone structure can also be subject to a neoplasm that by it very nature reduces the volume of the intracranial cavity, and can damage the brain.
By behavior of the neoplasm[edit]
Braintumors or intracanial neoplasms can be cancerous (malignant) or non-cancerous (benign), however the definitions of malignant or benign neoplasms differs from those commonly used in other types of cancerous or non-cancerous neoplasms in the body. In ordinary cancers (elsewhere in the body) three malignant properties differentiate benign tumors from malignant forms of cancer : benign tumors are self-limited and do not invade or metastasize. The malignant characteristics of tumors are :
- uncontrolled mitosis (growth by division beyond the normal limits),
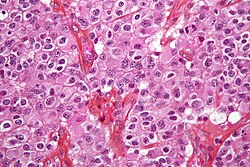
- Anaplasia is a way that cells change, anaplastic cells display marked pleomorphism. The cell nuclei are characteristically extremely hyperchromatic (darkly stained) and enlarged : the nucleus might have the same size as the cytoplasm of the cell (nuclear-cytoplasmic ratio may approach 1:1, instead of the normal 1:4 or 1:6 ratio). Giant cells that are considerably larger than their neighbors may be formed and possess either one enormous nucleus or several nuclei (syncytia). Anaplastic nuclei are variable and bizarre in size and shape.
- invasion or infiltration : in medical literature these terms are used as synonymous equivalents. However for clarity in the articles that follow we will adhere to a convention that they mean slightly different things(so readers should be aware that this convention is not kept outside these articles) :
- Invasion or invasiveness : is the spacial expansion of the tumor through the uncontrolled mitosis, in the sense that the neoplasm invades the space occupied by adjacent tissue, thereby pushing the other tissue aside and eventually compressing the tissue, often these tumors are associated with clearly outlined tumors in imaging.
- Inflitration : is the behavior of the tumor either to grow (microscopic) tentacles that push into the surrouding tissue (often making the outline of the tumor undefined or diffuse) or to have tumor cells "seeded" into the tissue beyond the circumference of the tumorous mass; this doesn't mean that an infiltrative tumor doesn't take up space or doesn't compress the surrounding tissue as it grows, but an infiltrating neoplasm makes it difficult to say where the tumor ends and the healthy tissue starts.
- metastasis (spread to other locations in the body via lymph or blood).
Of the above malignant characteristics some elements don't apply to primary neoplasms of the brain :
- Primary brain tumors don't metastasize to other organs, some forms of primary brain tumors can metastasize but will not spread outside the intracanial cavity or the central spinal canal.
- Primary brain tumors generally are invasive (ie. they will expand spatially and intrude into the space occupied by other brain tissue and compress those brain tissues), however some of the more malignent primary brain tumors will infiltrate the surrounding tissue.
Of numerous grading systems in use for the classification of tumor of the central nervous system, the World Health Organization (WHO) grading system is commonly used for astrocytoma. Established in 1993 in an effort to eliminate confusion regarding diagnoses, the WHO system established a four-tiered histologic grading guideline for astrocytomas that assigns a grade from 1 to 4, with 1 being the least aggressive and 4 being the most aggressive.
Tumor development according to tissuetype[edit]
Basic knowledge of the anatomy of the brain needed for further reading[edit]
From the brain-lemma we can learn a lot of things about the composition of the brain from different types of organic tissues. For the purpose of this article we will provide some summary notes only.

When reading the human brain in the picture on the left, only a few of the areas are realy of interest to us. The first type of tissue encounterd beneath the skullbone in the intracranial cavity is actually not shown on this picture : the meninges
Meninges[edit]
Human brains are surrounded by a system of connective tissue membranes called meninges that separate the skull from the brain. This three-layered covering is composed of (from the outside in) the dura mater ("hard mother"), arachnoid mater ("spidery mother"), and pia mater ("soft mother"). The arachnoid and pia are physically connected and thus often considered as a single layer, the pia-arachnoid. Below the arachnoid is the subarachnoid space which contains cerebrospinal fluid (CSF also called "liquor" in latin), which circulates in the narrow spaces between cells and through cavities called ventricles, and serves to nourish, support, and protect the brain tissue. Blood vessels enter the central nervous system through the perivascular space above the pia mater. The cells in the blood vessel walls are joined tightly, forming the blood-brain barrier which protects the brain from toxins that might enter through the blood. Tumors of the meninges are meningioma and are often benign neoplasms.
Brain matter[edit]
The brains of vertebrates (including humans) are made of very soft tissue, with a texture that has been compared to jello. Living brain tissue is pinkish on the outside and mostly white on the inside, with subtle variations in color
- the telencephalon (cerebral hemispheres or cerebrum)
- mesencephalon (midbrain),
- cerebellum
make out the biggest volume of the brain. These areas are composed of two broad classes of cells: neurons and glia. These two types are equally numerous in the brain as a whole, although glial cells outnumber neurons roughly 4 to 1 in the cerebral cortex. Glia come in several types, which perform a number of critical functions, including structural support, metabolic support, insulation, and guidance of development.
Primary tumors of the glialcells are called Glioma and often are malignant by the time they are diagnosed.
Spinal cord and other tissues[edit]
- the pink area in the picture is called the pons it's a specific region that consists of myelinated axons much like the spinal cord ;
- the yellow region is the diencephalon(thalamus and hypothalamus) which consist also of neuron and glialcell tissue with the hypophysis (or pituitary gland) attached at the bottom which is glandular tissue, tumors of the pituitary and pineal gland are often benign neoplasms;
- the turquoise region or medulla oblongata is the end of the spinal cord and is composed mainly of neuron tissue envelopped in Schwanncells and meninges tissue. Our spinal cord is made up of bundles of these axons. Glial cells such as Schwann cells in the periphery or, within the cord itself, oligodendrocytes, wrap themselves around the axon, thus promoting faster transmission of electrical signals and also providing for general maintenance of the environment surrounding the cord, in part by shuttling different compounds around, responding to injury, etc.
Brain tumors in infants and children[edit]

In the US, about 2000 children and adolescents younger than 20 years of age are diagnosed with malignant brain tumors each year. Higher incidence rates were reported in 1975–83 than in 1985–94. There is some debate as to the reasons; one theory is that the trend is the result of improved diagnosis and reporting, since the jump occurred at the same time that MRIs became available widely, and there was no coincident jump in mortality. The CNS cancer survival rate in children is approximately 60%. The rate varies with the type of cancer and the age of onset: younger patients have higher mortality.[1]
In children under 2, about 70% of brain tumors are medulloblastoma, ependymoma, and low-grade glioma. Less commonly, and seen usually in infants, are teratoma and atypical teratoid rhabdoid tumor.[2] Germ cell tumors, including teratoma, make up just 3% of pediatric primary brain tumors, but the worldwide incidence varies significantly.[3]
Schematic overview of tumors[edit]
Characteristics of tumors[edit]
Tumors have characteristics that allow pathologists to determine how dangerous a tumor is/was for the patient, how it will evolve and it will allow the medical team to determine the management plan for the patient.
Anaplasia : or dedifferentiation; loss of differentiation of cells and of their orientation to one another and blood vessels, a characteristic of anaplastic tumor tissue. Anaplastic cells have lost total control of their normal functions and many have deteriorated cell structures. Anaplastic cells often have abnormally high nuclear-to-cytoplasmic ratios, and many are multinucleated. Additionally, the nuclei of anaplastic cells are usually unnaturally-shaped or oversized nuclei. Cells can become anaplastic in two ways: neoplastic tumor cells can dedifferentiate to become anaplasias (the dedifferentiation causes the cells to lose all of their normal structure/function), or cancer stem cells can increase in their capacity to multiply (i.e., uncontrollable growth due to failure of differentiation).
Atypia: is an indication of abnormality of a cell (which may be indicative for malignancy). Significance of the abnormality is highly dependent on context.
Neoplasia: is the (uncontrolled division) of cells; as such neoplasia is not problematic but its consequences are: the uncontrolled division of cells means that the mass of a neoplasm increases in size, in a confined space such as the intracranial cavity this quickly becomes problematic because the mass invades the space of the brain pushing it aside, leading to compression of the brain tissue and increased intracranial pressure [4] and destruction of brain parenchyma. Increased Intracranial pressure (ICP) may be attributable to the direct mass effect of the tumor, increased blood volume, or increased cerebrospinal fluid (CSF) volume may in turn have secondary symptoms
Necrosis: is the (premature) death of cells, caused by external factors such as infection, toxin or trauma. Necrotic cells send the wrong chemical signals which prevents phagocytes from disposing of the dead cells, leading to a build up of dead tissue, cell debris an toxins at or near the site of the necrotic cells [5]
Arterial and venous hypoxia or the deprivation of adequate oxygen supply to certain areas of the brain, this is due to the fact that the tumor taps into nearby bloodvessels for its supply of blood, the neoplasm enters into competition for nutrients with the surrounding braintissue.
More generally a neoplasm may cause release of metabolic end products (eg, free radicals, altered electrolytes, neurotransmitters), release and recruitment of cellular mediators (eg, cytokines) that disrupt normal parenchymal function.
Signs and symptoms[edit]
The visibility of signs and symptoms of brain tumors mainly depends on two factors: tumor size (volume) and tumor location. The moment that symptoms will become apparent, either to the person or people around him (symptom onset) is an important milestone in the course of the diagnosis and treatment of the tumor. The symptom onset - in the timeline of the development of the neoplasm - depends in many cases on the nature of the tumor but in many cases it's also related to the change of the neoplasms nature from "benign" (i.e. slow-growing/late symptom onset) to more malignant(fast growing/early symptom onset) grading, and coincides frequently with the moment for seeking medical attention.
Symptoms of solid neoplasms of the brain (or primary brain tumors) can be devided is 3 main categories :
- Consequences of intracranial hypertension : The symptoms that often occur first are those that are the consequences of increased intracranial pressure: Large tumors or tumors with extensive perifocal swelling (edema) inevitably lead to elevated intracranial pressure (intracranial hypertension), which translates clinically into headaches, vomiting (sometimes without nausea), altered state of consciousness (somnolence, coma), dilatation of the pupil on the side of the lesion (anisocoria), papilledema (prominent optic disc at the funduscopic eye examination). However, even small tumors obstructing the passage of cerebrospinal fluid (CSF) may cause early signs of increased intracranial pressure. Increased intracranial pressure may result in herniation (i.e. displacement) of certain parts of the brain, such as the cerebellar tonsils or the temporal uncus, resulting in lethal brainstem compression. In very young children, elevated intracranial pressure may cause an increase in the diameter of the skull and bulging of the fontanelles.
- Dysfunction : depending on the tumor location and the damage it may have caused to surrounding brain structures, either through compression or infiltration, any type of focal neurologic symptoms may occur, such as cognitive and behavioral impairment (including impaired judgment, memory loss, lack of recognition, spatial orientation disorders), personality or emotional changes, hemiparesis, hypoesthesia, aphasia, ataxia, visual field impairment, impaired sense of smell, impaired hearing, facial paralysis, double vision, but more severe symptoms might accur too such as: paralysis on one side of the body hemiplegia or impairment to swallow . These symptoms are not specific for brain tumors — they may be caused by a large variety of neurologic conditions (e.g. stroke, traumatic brain injury). What counts, however, is the location of the lesion and the functional systems (e.g. motor, sensory, visual, etc.) it affects. A bilateral temporal visual field defect (bitemporal hemianopia—due to compression of the optic chiasm), often associated with endocrine disfunction—either hypopituitarism or hyperproduction of pituitary hormones and hyperprolactinemia is suggestive of a pituitary tumor.
- Irritation : signs abnormal fatigue, weariness, absences and tremors, but also [[epilepsy|epileptic seizures].
The above symptoms are true for ALL types of Neoplasm of the brain (i.e. that includes secondary tumors). It is very likely that a person might carry a primary benign neoplasme for several years and have no visible symptoms at all, or suffer no effects. Many present some vague an intermittent symptoms like headaches and occasional vomitting, and weariness which is easily mistaken for gastritis or gastroenteritis. If a person suffering from a metastasized cancer is diagnosed it wil be likely that a scan of the skull will be made and a secondary tumor discovered.
In a recent study by the Dutch GP Association [2], a list of causes of headaches [3] was published, that should alert GP's to take their diagnosis further then to choose for symptomatic treatment of headaches with simple pain medication (note the occurence of brain tumors as possible cause) :
| Alarm Signals | Possible Cause to be investigated |
|---|---|
| first headache complaint form patient over 50 | brain tumor, arteriïtis temporalis |
| first migaine attack in patient over 40 | brain tumor |
| headache from patient under 6 | hersentumor, hydrocephalus |
| senior patient with pain at temples | arteriïtis temporalis |
| pregnancy with unknown headache | pre-eclampsie |
| increased headaches after trauma | sub/epiduraal hematoma |
| high-pitched headaches with high bloodpressure | malign hypertension |
| acute high pitched headache | meningitis, CVA (Cerebrovascular accident or stroke), subarachnoïdale hemorrage |
| headache and fever (with reduced consciencesness) | meningitis |
| Stiffness of the neck/neurological dysfunction | meningitis, brain tumor |
| headache with signs of elevated intracranial pressure | brain tumor |
| focal neurological dysfunction | brain tumor |
| early morning vomitting or vomitting unrelated to headache | brain tumor |
| behavioural changes or rapid decline in school results | brain tumor |
| aura migraine always at one side | brain tumor |
Diagnosis[edit]
Although there is no specific or singular clinical symptom or sign for any brain tumors, the presence of a combination of symptoms and the lack of corresponding clinical indications of infections might be an indicator to step up the diagnostic investigation to the direction of an intracranial neoplasm.
The diagnosis will often start with an interrogation of the patient to get a clear view of his medical antecedents, and his current symptoms. Clinical and laboratory investigations will serve to exclude infections as cause of the symptoms. Examinations in this stage may include ophtamological, otolaryngological (or ENT) and/or Electrophysiological exams, other means such as electroencephalography (EEG) play a role in the diagnosis of brain tumors.
Swelling, or obstructing the passage of cerebrospinal fluid (CSF) may cause (early) signs of increased intracranial pressure which translates clinically into headaches, vomiting, or an altered state of consciousness, (and in children) changes to the diameter of the skull and bulging of the fontanelles. More complex symptoms such as endocrine disfunctions should alarm doctors not to exclude braintumors.
A bilateral temporal visual field defect (due to compression of the optic chiasm) or dilatation of the pupil, and the occurrance of either slowly evolving or the sudden onset of focal neurologic symptoms, such as cognitive and behavioral impairment (including impaired judgment, memory loss, lack of recognition, spatial orientation disorders), personality or emotional changes, hemiparesis, hypoesthesia, aphasia, ataxia, visual field impairment, impaired sense of smell, impaired hearing, facial paralysis, double vision, but also more severe symptoms might accur too such as: tremors, paralysis on one side of the body hemiplegia, but also (epileptic) seizures in a patient with a negative history for epilepsy, impairment to swallow should raise red flags
Imaging plays a central role in the diagnosis of brain tumors. Early imaging methods —invasive and sometimes dangerous— such as pneumoencephalography and cerebral angiography, have been abandoned in recent times in favor of non-invasive, high-resolution techniques, such as computed tomography (CT)-scans and especially magnetic resonance imaging (MRI). Neoplasms will often show as differently coloured masses (also referred to as processes) in CT or MRI results.
- Benign brain tumors often show up as hypodense (darker than brain tissue) mass lesions on cranial CT-scans. On MRI, they appear either hypo- (darker than brain tissue) or isointense (same intensity as brain tissue) on T1-weighted scans, or hyperintense (brighter than brain tissue) on T2-weighted MRI, although the appearance is variable.
- Contrast agent uptake, sometimes in characteristic patterns, can be demonstrated on either CT or MRI-scans in most malignant primary and metastatic brain tumors.
- Perifocal edema , or pressure-areas, or where the brain tissue has been compressed by an invasive process also appears hyperintense on T2-weighted MRI, they might indicate the presence a diffuse neoplasm (unclear outline)
This is because these tumors disrupt the normal functioning of the blood-brain barrier and lead to an increase in its permeability. However it is not possible to diagnose high versus low grame gliomas based on enhancement pattern alone.
Another possible diagnostic indicator would be neurofibromatosis which can be in type one or type two.
Glioblastoma multiforme and anaplastic astrocytoma have been associated in case reports on PubMed[who?] with the genetic acute hepatic porphyrias (PCT, AIP, HCP and VP), including positive testing associated with drug refractory seizures. Unexplained complications associated with drug treatments with these tumors should alert physicians to an undiagnosed neurological porphyria.
The definitive diagnosis of brain tumor can only be confirmed by histological examination of tumor tissue samples obtained either by means of brain biopsy or open surgery. The histological examination is essential for determining the appropriate treatment and the correct prognosis. This examination, performed by a pathologist, typically has three stages: interoperative examination of fresh tissue, preliminary microscopic examination of prepared tissues, and followup examination of prepared tissues after immunohistochemical staining or genetic analysis.
Treatment[edit]
When a braintumor is diagnosed a medical team will be formed to assess the options of treatment presented by the leading suregon to the patient and his family. Given the location of primary solid neoplasms of the brain in most cases there is no "do-nothing" option, neurosurgeons do take the time to observe the evolution of the neoplasm before proposing a management plan to the patient and his relatives. Different types of treatment are available to the doctors and can be combined to give the the best chances of survival :
- surgery : complete or partial ressection of the tumor ; objective : to remove as many tumor cells as possible
- radiotherapy
- chemotherapy
- kill as many as possible of the cells left behind
- put remaining tumor cells into a nondividing, sleeping state for as long as possible
Survival rates in primary brain tumors depend on the type of tumor, age, functional status of the patient, the extent of surgical tumor removal, to mention just a few factors.[6]
Surgery[edit]
The primary course of action described in medical literature is surgical removal (ressection), a craniotomy(to open the skull) to best access the tumor site, currently minimal invasive techniques are being studied but far form being common practise. The prime remediating objective of surgery is to remove as many tumorcells as possible, in any case surgery will reduce the tumor size and will attempt to completely remove the neoplasm. In some cases access to the tumor is impossible and impedes surgery.
Many meningiomas, with the exception of some tumors located at the skull base, can be successfully removed surgically. Most pituitary adenomas can be removed surgically, often using a minimally invasive approach through the nasal cavity and skull base (trans-nasal, trans-sphenoidal approach). Large pituitary adenomas require a craniotomy (opening of the skull) for their removal. Radiotherapy, including stereotactic approaches, is reserved for the inoperable cases.
Although there is no generally accepted therapeutic management for primary brain tumors, a surgical attempt at tumor removal or at least cytoreduction (that is, removal of as much tumor as possible, in order to reduce the number of tumor cells available for proliferation) is considered in most cases.[7] However, due to the infiltrative nature of these lesions, tumor recurrence, even following an apparently complete surgical removal, is not uncommon. Several current research studies aim to improve the surgical removal of brain tumors by labeling tumor cells with a chemical (5-aminolevulinic acid) that causes them to fluoresce [8]. Postoperative radiotherapy and chemotherapy are integral parts of the therapeutic standard for malignant tumors. Radiotherapy may also be administered in cases of "low-grade" gliomas, when a significant tumor burden reduction could not be achieved surgically.
The main treatment option for single metastatic tumors is surgical removal, followed by radiotherapy and/or chemotherapy. Multiple metastatic tumors are generally treated with radiotherapy and chemotherapy. Stereotactic radiosurgery (SRS), such as Gamma Knife, Cyberknife or Novalis Tx, radiosurgery, remains a viable option. However, the prognosis in such cases is determined by the primary tumor, and it is generally poor.
Radiation therapy[edit]
The goal of radiation therapy is to selectively kill tumor cells while leaving normal brain tissue unharmed. In standard external beam radiation therapy, multiple treatments of standard-dose "fractions" of radiation are applied to the brain. Each treatment induces damage to both healthy and normal tissue. By the time the next treatment is given, most of the normal cells have repaired the damage, but the tumor tissue has not. This process is repeated for a total of 10 to 30 treatments, depending on the type of tumor. This additional treatment provides some patients with improved outcomes and longer survival rates.
Radiosurgery is a treatment method that uses computerized calculations to focus radiation at the site of the tumor while minimizing the radiation dose to the surrounding brain. Radiosurgery may be an adjunct to other treatments, or it may represent the primary treatment technique for some tumors.
Radiotherpy may be used if there is incomplete resection of the tumor. Forms of radiotherapy used for brain cancer include external beam radiation therapy, brachytherapy ,and in more difficult cases, stereotactic radiosurgery, such as Gamma knife, Cyberknife or Novalis Tx radiosurgery, remains a viable option.[9]
Radiotherapy is the most common treatment for secondary cancer brain tumors. The amount of radiotherapy depends on the size of the area of the brain affected by cancer. Conventional external beam whole brain radiotherapy treatment (WBRT) or 'whole brain irradiation' may be suggested if there is a risk that other secondary tumors will develop in the future.[10] Stereotactic radiotherapy is usually recommended in cases of under three small secondary brain tumors.
In 2008 a study published by the University of Texas M. D. Anderson Cancer Center indicated that cancer patients who receive stereotactic radiosurgery (SRS) and whole brain radiation therapy (WBRT) for the treatment of metastatic brain tumors have more than twice the risk of developing learning and memory problems than those treated with SRS alone.[11][12]
Chemotherapy[edit]
Patients undergoing chemotherapy are administered special drugs designed to kill tumor cells. Although chemotherapy may improve overall survival in patients with the most malignant primary brain tumors, it does so in only about 20 percent of patients. Chemotherapy is often used in young children instead of radiation, as radiation may have negative effects on the developing brain. The decision to prescribe this treatment is based on a patient’s overall health, type of tumor, and extent of the cancer. The toxicity, the many side effects and the uncertain outcome of chemotherapy in braintumors puts this treatment further down the line op treatment options for medical teams.
UCLA Neuro-Oncology publishes real-time survival data for patients with this diagnosis. They are the only institution in the United States that shows how brain tumor patients are performing on current therapies. They also show a listing of chemotherapy agents used to treat high grade glioma tumors.
A shunt operation is used not as a cure but to relieve the symptoms.[4] The hydrocephalus caused by the blocking drainage of the cerebrospinal fluid can be removed with this operation.
Researchers are presently investigating a number of promising new treatments including gene therapy, highly focused radiation therapy, immunotherapy and novel chemotherapies. A number of new treatments are being made available on an investigational basis at centers specializing in brain tumor therapies.
Research to treatment with the vesicular stomatitis virus[edit]
In 2000, researchers at the University of Ottawa, led by John Bell PhD., have discovered that the vesicular stomatitis virus, or VSV, can infect and kill cancer cells, without affecting healthy cells if coadministered with interferon.[13]
The initial discovery of the virus' oncolytic properties were limited to only a few types of cancer. Several independent studies have identified many more types susceptible to the virus, including glioblastoma multiforme cancer cells, which account for the majority of brain tumors.
In 2008, researchers artificially engineered strains of VSV that were less cytotoxic to normal cells. This advance allows administration of the virus without coadministration with interferon. Consequently administration of the virus can be given intravenously or through the olfactory nerve. In the research, a human brain tumor was implanted into mice brains. The VSV was injected via their tails and within 3 days all tumor cells were either dead or dying.[citation needed][dubious ]
Research on virus treatment like this has been conducted for some years, but no other viruses have been shown to be as efficient or specific as the VSV mutant strains. Future research will focus on the risks of this treatment, before it can be applied to humans.[14]
Consequences for survivors[edit]
As was pointed out above the presence of a braintumor is a very critical and life threatening situation. The discovery of a braintumor (except the lowgraded primary tumors) starts medically speaking a race against time.
The consequences - and chances of survival - of the treatment of secondary tumors (metastasis of other cancers) are hard to predict as its depends on the type and evolution of the treatment of the primary tumor, and to what extend a patient responds to treatment.
The consequences of treatment of primary tumors however is a totally different matter. Survival of the treatment of a (solid) neoplasm of the brain (and central nervous system) has dramatically increased over the yearsalso for the higher graded tumors, also long term survival of younger patients is on the increase.
Patients with benign gliomas may survive for many years,[15][16] while survival in most cases of glioblastoma multiforme is limited to a few months after diagnosis if treatment is ignored (do nothing option), but cases are know of glioblastoma multiforme that have survived over 20 years and have a good quality of life after successful treatment, even after repeated treatment of early diagnosed recidive of a tumerous process.
After surgical treatment the medical team might decide further post-operative treatment with Radiotherapy and/or Chemotherapy. There are some adverse affects of these treatments but considering the impact of a brain tumor the loss of hair has mostly a cosmetic and psychological effect. Nausea is a well known side effect of chemotherapy that should be mo nitored and regulary reported to the medical team in an out-patient situation. Family members should be aware that whilst the radiotherapy is ongoing healing of (external)surgery wounds in the area of the therapy is strongly influenced, in such case have the nurses monitor the evolution of such wounds daily after each radiotherapy session. Superficial infection might get hold of the wound if crae is ont given professionally.
Physical consequences[edit]
After surgery patients need time to recover physically. The first hurdles to take for the patient, after being released form the IC-unit and his vital signs are stable, are :
- swallow reflex
- movement of limbs and detailed movements (fingers)
- being able to stand and equilibrium
Things that might go wrong in this phase of recovery is (partial) paralysis, incontinence, tremors and seizures(see below epileptic seizures), some of these effects are temporal, and might be overcome with rehabilitation.
Its important for family members to know that patients suffer a huge loss in weight and muscular mass. Small efforts like walking to the toilet will be an important physical effort, and walking from their hospital bed to a patient-family lounge or to the frontdoor of the hospital will cause the patient to be tired. Rebuilding physical strength, some basic endurance and resistance will be a process of months even years even for previously well-trained athletes. The medical team will help you (teh patient and the family) with training programs when the time is right for such programs.
Impact on the daily life of the family[edit]
After initial surgery when the patient returns to the home situation, they shouldn't be left unsupervised at all, your medical team will advise when the patient has regained enough independance to be left alone. Medication should be given at a strict regime nurse and your medical team will advise on how strict/flaxible this should be adhered to. Keep a medical diary and note :
- when medication is given (time, quantity)
- read fever/temperature at least twice a day (and everytime fever is suspected)
- read heartrate and bloodpressure every day
- note when nausea and pain is experienced
- note any situation out of the ordinary (pus coming out of a wound etc..), swelling etc
Your life will - from the release form hospital onward - be regulated by the clock of the braintumor patient medication and regular visits for check-ups.
Epileptic seizures[edit]
Any person undergoing brain surgery may suffer from epileptic seizures. Seizures can vary from absences to severe tonic-clonic attacks. Medication is prescribed and administered to minimize, eliminate the occurence of seizures. Parents of children, family members of adults and relatives in general of patients that have undergone surgery to remove a brain tumor, and who haven't got the benefit of medical education or experience should be made aware of this fact. Experiences in patient-family support groups learn that they are informed but are actually totally unprepared for the occurence of an Tonic-clonic_seizure.
From personal experience this example: We were informed both by medical staff and by leaflets from family-support associations that our son could have epileptic seizure(s) as a consequence of the surgery, this forewarning wasn't sufficient. I had previously witnessed a few (tonic-clonic) epileptic seizures from epilepsy-patients under medication. Those patients would fall to the ground have some muscle spams, and after a few minutes this would calm down, they would regain conscienceness, feel somewhat disoriented, get up and sit down on their chair as if they returned from the bathroom. On a scale of 1-10 such an attack would scale in at about 1 or at the utmost 2. As a bystander I just knew I had to free the throat-area from restricting clothing that would hinder respiration, and make sure the person having the attack would not hurt himself on furniture standing around. But when my son had a tonic-clonic seizure, just weeks after his surgery, I was totally unprepared. The first attack would be rated 4 or 5 at that scale mentionned before. Several tonic-clonic seizures, increasing in amplitude follow each other in a rapid tempo, within 10 minutes he underwent his 3rd attack without regaining conscienceness between the seizures, the 3rd attack could easily be rated 8. It was impossible to determine wether he had a heartbeat, or wether he was breathing, his skin colour turned grayish. I wasn't sure if i was doing enough to make sure he could continue to breath. I called in the emergency services. They dispatched a cardiac-ambulance unit and a emergency medical team (ER-doctor) and even with 4 staff I could still offer help (even if i was only holding the perfusion bag at one stage). Thanks to medication (intravenous valium) the next attack was calmed down in amplitude but continued for perhaps as long as 30 minutes. Only after more then 2 hours my son regained some form of conscienceness, enabling him to respond to what we were saying. I think relatives should get video-based or multimedia training that prepares them to what they will experience during epileptic seizure and how they should respond to the situation. [17]
The level of anti-epilepsy medication varies from patient to patient and depends on the severity of the lesion. So the doctors have to experiment to determine the applicable level of medication, this could cause some more or less severe epileptic seizures, relatives in care of people recovering form surgery might find the first aid section useful reading.
Psychological and behavioural consequences[edit]
It might be very difficult to communicate at first with the patient, and family often will see that reaction isn't forthcoming or response comes very slow. This is perfectly normal and will wear off while the patient recovers, we might be talking weeks or months. At first family members might have to interpret answers like "yes", "no" and the tone of patient's grunts get an idea of the patients reaction. Friends coming to visit a patient might find him unresponsive or staring at the TV-screen. This is normal behaviour, as the patient gets to grips with his condition he will learn to talk in phrases again and to express his ideas an feelings again, but in the beginning he will have difficulty finding the words to describe his feelings. In soem cases patients might be react uninhibitedly towards some social conventions, they are not aware of that behaviour and you should seek specialist help, in order to avoid adverse reactions towards caring relatives. If the reaction is verbal respond normaly even if the reaction is negative, if the reaction is physical correct it, in any case react as if the patients action was normal within the social convention without shaming or punishing. Don't ignore or pretend as if nothing happened but seek professional help with your psychologist who can tell you how to respond and when its time to retrain this social conventional behaviour.
Occurence of Brain tumors[edit]
International The incidence of low-grade astrocytoma has not been shown to vary significantly with nationality. However, studies examining the incidence of malignant CNS tumors have shown some variation with national origin. Since some of these high-grade lesions arise from low-grade tumors, these trends are worth mentioning. Specifically, the incidence of CNS tumors in the United States, Israel, and the Nordic countries is relatively high, while Japan and Asian countries have a lower incidence. These differences probably reflect some biological differences as well as differences in pathologic diagnosis and reporting.[18]
Worlwide figures[edit]
Worldwide data on incidence of cancer can be found at the WHO (world health organisation) and is handled by the AIRC (Agency for Interanctional Research on Cancer) located in France. [5], following tables were extracted from the online database GloboCancer :
- Regional Summary of Occurence of cancers of the Brain & nervous system in Women,
- Regional Summary of Occurence of cancers of the Brain & nervous system in Men,
- Country based Incidence Rate of cancers of the Brain & nervous system in Women,
- Country based Incidence Rate of cancers of the Brain & nervous system in Men
Some conclusions can be drawn from these figures. Figures for incidences of cancers of the brain show a significant difference between more and less developped countries (i.e. the lesser developped countries have less incidences of tumors of the brain) this should be explained by undiagnosed tumorrelated deaths (patient in extreem poor situations don't get diagnosed simply because they don't get in touch with the modern diagnostic facilities required to diagnose a braintumor) and by deaths caused by other poverty related causes that pre-empt a patients life before tumors develop or tumors become life threatening. Nevertheless studies have ben made that certain forms of primary brain tumors are more prevalent among certain groups of the population.
National figures[edit]
From the British national statistics dat about new diagnosis of maglignant neoplasms of the brain for the year 2007 (in absolute figures and in rates per 100.000)
ICD-10 code : C71 Description : Malignant neoplasm of brain
| Gender | DASR | All ages | Under 1 | 1-4 | 5-9 | 10-14 | 15-19 | 20-24 | 25-29 | 30-34 | 35-39 | 40-44 | 45-49 | 50-54 | 55-59 | 60-64 | 65-69 | 70-74 | 75-79 | 80-84 | 85+ |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Absolute figures | |||||||||||||||||||||
| M | 2.130 | 7 | 34 | 39 | 31 | 37 | 33 | 48 | 61 | 87 | 100 | 116 | 142 | 242 | 264 | 258 | 237 | 193 | 128 | 73 | |
| F | 1.598 | 7 | 42 | 39 | 37 | 28 | 25 | 37 | 50 | 42 | 73 | 87 | 99 | 140 | 191 | 166 | 169 | 158 | 111 | 97 | |
| Rates per 100.000 inhabitants | |||||||||||||||||||||
| M | 7,7 | 8,5 | 2,1 | 2,8 | 2,7 | 2,0 | 2,1 | 1,9 | 2,8 | 3,7 | 4,6 | 5,1 | 6,6 | 9,3 | 15,7 | 18,6 | 24,0 | 25,8 | 26,7 | 26,6 | 21,2 |
| F | 5,3 | 6,2 | 2,2 | 3,6 | 2,8 | 2,5 | 1,7 | 1,5 | 2,2 | 3,0 | 2,2 | 3,7 | 4,9 | 6,3 | 8,8 | 12,9 | 14,3 | 16,2 | 17,1 | 15,1 | 12,8 |
GB Office National statistics , online http://www.statistics.gov.uk/downloads/theme_health/2007cancerfirstrelease.xls
CBTRUS (Central Brain Tumor Registry of the United States),
In the United States in the year 2005, it was estimated there were 43,800 new cases of brain tumors (Central Brain Tumor Registry of the United States, Primary Brain Tumors in the United States, Statistical Report, 2005–2006),[19] which accounted for 1.4 percent of all cancers, 2.4 percent of all cancer deaths,[20] and 20–25 percent of pediatric cancers.[20][21] Ultimately, it is estimated there are 13,000 deaths per year in the United States alone as a result of brain tumors.[19]
Notes[edit]
See also[edit]
- Craterization
- List of notable brain tumor patients
- Radiosurgery
- Stereotactic surgery
- Radiation therapy
- Grading of the tumors of the central nervous system
- Visualase
References[edit]
- ^ Gurney, James G. "CNS and Miscellaneous Intracranial and Instraspinal Neoplasms" (PDF). SEER Pediatric Monograph. National Cancer Institute. pp. 51–52 (incidence), pp. 56–57 (trends), p. 57 (survival). Retrieved 4 December 2008.
[re incidence] In the US, approximately 2,200 children and adolescents younger than 20 years of age are diagnosed with malignant central nervous system tumors each year. More than 90 percent of primary CNS malignancies in children are located within the brain.
{{cite web}}: Unknown parameter|coauthors=ignored (|author=suggested) (help) - ^ Infantile Brain Tumors by Brian Rood for The Childhood Brain Tumor Foundation (accessed July 2007)
- ^ Echevarría ME, Fangusaro J, Goldman S (June 2008). "Pediatric central nervous system germ cell tumors: a review". Oncologist. 13 (6): 690–9. doi:10.1634/theoncologist.2008-0037. PMID 18586924. S2CID 8114229.
{{cite journal}}: CS1 maint: date and year (link) CS1 maint: multiple names: authors list (link) - ^ http://www.helium.com/items/1354248-difference-between-metaplasia-heteroplasia-dysplasia-neoplasia-hyperplasia-anaplasia
- ^ http://www.nlm.nih.gov/medlineplus/ency/article/002266.htm
- ^ Nicolato A, Gerosa MA, Fina P, Iuzzolino P, Giorgiutti F, Bricolo A (Sep 1995). "Prognostic factors in low-grade supratentorial astrocytomas: a uni-multivariate statistical analysis in 76 surgically treated adult patients". Surg Neurol. 44 (3): 208–21, discussion 221–3. doi:10.1016/0090-3019(95)00184-0. PMID 8545771.
{{cite journal}}: CS1 maint: date and year (link) CS1 maint: multiple names: authors list (link) - ^ Nakamura M, Konishi N, Tsunoda S (Feb 2000). "Analysis of prognostic and survival factors related to treatment of low-grade astrocytomas in adults". Oncology. 58 (2): 108–16. doi:10.1159/000012087. PMID 10705237. S2CID 25943854.
{{cite journal}}: CS1 maint: date and year (link) CS1 maint: multiple names: authors list (link) - ^ Clinical trials in brain tumors.. Accessed June 2000.
- ^ Radiosurgery treatment comparisons - Cyberknife, Gamma knife, Novalis Tx
- ^ Treating secondary brain tumours with WBRT
- ^ Whole Brain Radiation increases risk of learning and memory problems in cancer patients with brain metastases
- ^ IRSA - International RadioSurgery Association - Metastatic brain tumors
- ^ Researchers Find Cancer-Killing Virus; July 24, 2000.
- ^ Yale Lab Engineers Virus That Can Kill Deadly Brain Tumors; February 21, 2008.
- ^ Janny P, Cure H, Mohr M (Apr 1994). "Low grade supratentorial astrocytomas. Management and prognostic factors". Cancer. 73 (7): 1937–45. doi:10.1002/1097-0142(19940401)73:7<1937::AID-CNCR2820730727>3.0.CO;2-G. PMID 8137221. S2CID 34884141.
{{cite journal}}: CS1 maint: date and year (link) CS1 maint: multiple names: authors list (link) - ^ Piepmeier J, Christopher S, Spencer D (May 1996). "Variations in the natural history and survival of patients with supratentorial low-grade astrocytomas". Neurosurgery. 38 (5): 872–8, discussion 878–9. doi:10.1097/00006123-199605000-00002. PMID 8727811.
{{cite journal}}: CS1 maint: date and year (link) CS1 maint: multiple names: authors list (link) - ^ this is an anonimised interview that relates a personal experience recorded in a patient-support group by ~~~~
- ^ George I Jallo, MD, & Ethan A Benardete, MD, PhD (januari 2010). [[1] "Low-Grade Astrocytoma"].
{{cite journal}}: Check|url=value (help); Check date values in:|date=(help); Cite journal requires|journal=(help)CS1 maint: date and year (link) CS1 maint: multiple names: authors list (link) - ^ a b Greenlee RT, Murray T, Bolden S, Wingo PA (2000). "Cancer statistics, 2000". CA Cancer J Clin. 50 (1): 7–33. doi:10.3322/canjclin.50.1.7. PMID 10735013. S2CID 26315886.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - ^ a b American Cancer Society. Accessed June 2000.
- ^ Chamberlain MC, Kormanik PA (Feb 1998). "Practical guidelines for the treatment of malignant gliomas". West J Med. 168 (2): 114–20. PMC 1304839. PMID 9499745.
{{cite journal}}: CS1 maint: date and year (link)
External links[edit]
- UWOBrain tumors, Approach to..
- Management Neuro-oncology disorders
- Brain Cancer Vaccine Video
- The Brain Tumor Trials Collaborative: Brain Tumor Research
- Brain and CNS cancers at Curlie
- WebMD: Brain Cancer Health Center
- Medical Image Database MR and CT Scans of Brain Tumors
- Seattle's Ivy Center for Advanced Brain Tumor Treatment
- Medical Encyclopedia MayoClinic: Brain tumor
- Brain Tumor: Definitions Neurosurgery UCLA
- Medline Plus: Brain Cancer – Interactive Health Tutorials
- Visualase Laser Technology For Thermal Tumor Ablation
- Brain Tumor Locations Differential Diagnosis
- MedPix Teaching File MR Scans of Primary Brain Lymphoma
