User:Dep003/sandbox
 | |
 | |
| Clinical data | |
|---|---|
| Trade names | Dilantin |
| AHFS/Drugs.com | Monograph |
| MedlinePlus | a682022 |
| Routes of administration | Oral, parenteral |
| ATC code | |
| Legal status | |
| Legal status |
|
| Pharmacokinetic data | |
| Bioavailability | 70-100% oral, 24.4% for rectal and intravenous administration |
| Protein binding | 90% |
| Metabolism | hepatic |
| Elimination half-life | 6–24 hours |
| Excretion | Primarily through the bile, urinary |
| Identifiers | |
| |
| CAS Number | |
| PubChem CID | |
| DrugBank | |
| ChemSpider | |
| UNII | |
| KEGG | |
| ChEBI | |
| ChEMBL | |
| Chemical and physical data | |
| Formula | C15H12N2O2 |
| Molar mass | 252.268 g/mol g·mol−1 |
| 3D model (JSmol) | |
| |
| |
| | |
Phenytoin sodium /fəˈnɪtoʊ[invalid input: 'ɨ']n/ is an antiepileptic drug used primarily in the management of complex partial seizures and generalized tonic-clonic seizures. Phenytoin is also used to prevent seizures following neurosurgery.[1] Phenytoin is believed to protect against seizures by causing voltage-dependent block of voltage-gated sodium channels.[2] Additionally, phenytoin is a class 1b antiarrhythmic that can be used to treat cardiac arrhythmias when conventional options have failed or after cardiac glycoside intoxication.[3]
Trade names[edit]
Phenytoin sodium has been marketed as Phenytek by Mylan Laboratories, previously Bertek Pharmaceuticals, and Dilantin; Australia also Dilantin Kapseals and Dilantin Infatabs in the USA, Eptoin by Abbott Group in India and as Epanutin in the UK and Israel, by Parke-Davis, now part of Pfizer. In the USSR and post-USSR countries, it was/is marketed as Дифенин (Diphenin, Dipheninum). FENTOIN-ER,EPSOLIN are brands available in India [4] Diphantoine is a brand available in The Netherlands (91% Phenytoin).
History[edit]
Phenytoin (diphenylhydantoin) was first synthesized by German chemist Heinrich Biltz in 1908.[5] Biltz sold his discovery to Parke-Davis, which did not find an immediate use for it. In 1938, outside scientists including H. Houston Merritt and Tracy Putnam discovered phenytoin's usefulness for controlling seizures, without the sedative effects associated with phenobarbital.
According to Goodman and Gilman's Pharmacological Basis of Therapeutics,
- In contrast to the earlier accidental discovery of the antiseizure properties of bromide and phenobarbital, phenytoin was the product of a search among nonsedative structural relatives of phenobarbital for agents capable of suppressing electroshock convulsions in laboratory animals.[6]
Jack Dreyfus, founder of the Dreyfus Fund, became a major proponent of phenytoin as a means to control nervousness and depression when he received a prescription for Dilantin in 1966. He is believed to have supplied large amounts of the drug to Richard Nixon throughout the late 1960s and early 1970s. Dreyfus' experience with phenytoin is outlined in his book, A Remarkable Medicine Has Been Overlooked.[7] Despite more than $70 million in personal financing, his push to see phenytoin evaluated for alternative uses has had little lasting effect on the medical community. This was partially because Parke-Davis was reluctant to invest in a drug nearing the end of its patent life, and partially due to mixed results from various studies. It was approved by the USA Food and Drug Administration in 1953 for use in seizures.
In 2008, the drug was put on the FDA's Potential Signals of Serious Risks List to be further evaluated for approval. The list identifies medications that the FDA has identified a potential safety issue, but does not mean that FDA has identified a causal relationship between the drug and the listed risk. To address this concern, the Warnings and Precautions section of the labeling for Dilantin injection was updated to include additional information about purple glove syndrome in November 2011.[8]
Mechanism of action[edit]
Phenytoin produces its anticonvulsant activity through blocking sustained high frequency repetitive firing of action potentials. This is accomplished by reducing the amplitude of sodium-dependent action potentials through enhancing steady state inactivation. Sodium channels exist in three main conformations 1.Resting state 2.Open state 3.Inactive state
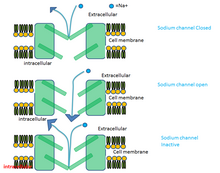
Phenytoin binds preferentially to the inactive form of the sodium channel. Because it takes time for the bound drug to dissociate from the inactive channel, there is a time dependent block of the channel. Since the fraction of inactive channels is increased by membrane depolarization as well as by repetitive firing, the binding to the inactive state by phenytoin sodium can produce voltage-dependent, use-dependent and time-dependent block of sodium-dependent action potentials. [9]
The primary site of action appears to be the motor cortex where spread of seizure activity is inhibited. Possibly by promoting sodium efflux from neurons, phenytoin tends to stabilize the threshold against hyperexcitability caused by excessive stimulation or environmental changes capable of reducing membrane sodium gradient. This includes the reduction of post-tetanic potentiation at synapses which prevents cortical seizure foci from detonating adjacent cortical areas. Phenytoin reduces the maximal activity of brain stem centers responsible for the tonic phase of generalized tonic-clonic seizures.[10]
Pharmacology[edit]
Phenytoin elimination kinetics show mixed-order behaviour at therapeutic concentrations. A small increase in dose may lead to a large increase in drug concentration as elimination becomes saturated. The time to reach steady state is often longer than 2 weeks.[11][12][13][14]
Use[edit]
- Grand mal - Abolishes grand mal seizure in nearly 60% of the patient and reduces their severity and frequency in another 15-20%. Dose: 100 mg twice daily, 400 mg/day maximum dose, children 5–8 mg/kg/day.
- Partial seizures - Phenytoin is preferred to phenobarbital in this type of seizure. The drug often controls but does not completely abolish the seizure activity. It is occasionally useful in infantile spasm.
- Status epilepticus
- Cardiac dysrhythmia
- Trigeminal neuralgia - Second choice drug to carbamazepine.[15]
- Although controversial,[16] but topical Phenytoin has been used as wound healing agent in patients with chronic skin wounds.[17][18][19][20]
Side-effects[edit]
Neurologic[edit]
At therapeutic doses, phenytoin may produce horizontal gaze nystagmus. At toxic doses, patients experience vertical nystagmus, sedation, cerebellar ataxia, and ophthalmoparesis, as well as seizures. Idiosyncratic side-effects of phenytoin, as with other anticonvulsants, include rash and severe allergic reactions.
Phenytoin may accumulate in the cerebral cortex over long periods of time, as well as causing atrophy of the cerebellum when administered at chronically high levels. Despite this, the drug has a long history of safe use, making it one of the more popular anti-convulsants prescribed by doctors, and a common "first line of defense" in seizure cases.
Hematologic[edit]
It has been suggested that phenytoin causes a reduction in folic acid levels, predisposing patients to megaloblastic anemia. Folic acid is presented in foods as polyglutamate, which is then converted into monoglutamates by intestinal conjugase. Phenytoin acts by inhibiting this enzyme, thereby causing folate deficiency.[21] Other side effects may include: agranulocytosis, aplastic anemia, leukopenia[citation needed], thrombocytopenia. [22]
Teratogenicity[edit]
Phenytoin is a known teratogen. The syndrome consists of craniofacial anomalies (broad nasal bridge, cleft lip and palate, microcephaly) and a mild form of mental retardation (average IQ=71).[23] This syndrome resembles the well-described Fetal Alcohol Syndrome[24] and has also been called the "fetal hydantoin syndrome". Some recommend avoiding polytherapy and maintaining the minimal dose possible during pregnancy, but acknowledge that current data do not provide clear answers.[25] Data now being collected by the Epilepsy and Antiepileptic Drug Pregnancy Registry may one day answer this question definitively.
Carcinogenicity[edit]
There is no good evidence that phenytoin is a human carcinogen.[26][27]
Gingival[edit]
Phenytoin has been associated with drug-induced gingival enlargement (overgrowth of the gums), probably due to above-mentioned folate deficiency; indeed, evidence from a randomized controlled trial suggests that folic acid supplementation can prevent gingival enlargement in children who take phenytoin.[28] Plasma concentrations needed to induce gingival lesions have not been clearly defined. Effects consist of the following: bleeding upon probing, increased gingival exudate, pronounced gingival inflammatory response to plaque levels, associated in some instances with bone loss but without tooth detachment.
Suicide risk[edit]
Following almost 200 studies of 11 anti-seizure drugs the FDA has also warned of an increased suicide risk for any patients treated with certain anti-seizure drugs. The study of 44,000 patients found that patients whose epilepsy is treated with drugs face about twice the risk of suicidal thoughts compared to placebo-takers. Although phenytoin was not named in the study, the FDA announced that it expected the risk applied to every epilepsy drug.[29]
Dermatologic[edit]
Hypertrichosis, rash, exfoliative dermatitis, pruritis, hirsutism, and coarsening of facial features
In autoimmune disease[edit]
Phenytoin has been known to cause drug-induced lupus.[30]
Phenytoin therapy has been linked to the life-threatening skin reactions Stevens–Johnson syndrome (SJS) and toxic epidermal necrolysis (TEN). These conditions are significantly more common in patients with a particular HLA-B allele, HLA-B*1502.[31] This allele occurs almost exclusively in patients with ancestry across broad areas of Asia, including South Asian Indians.
In immunodeficiency disease[edit]
Phenytoin is also associated with induction of reversible IgA deficiency.[31]
Interactions[edit]
A 1981 study [32] by the National Institutes of Health showed that antacids administered concomitantly with phenytoin "altered not only the extent of absorption but also appeared to alter the rate of absorption. Antacids administered in a peptic ulcer regimen may decrease the AUC of a single dose of phenytoin. Patients should be cautioned against concomitant use of antacids and phenytoin."
Phenytoin is an inducer of the CYP3A4 and CYP2C19 families of the P450 enzyme responsible for the hepatic degradation of various drugs.
Warfarin (Coumadin) and Trimethoprim increase serum phenytoin levels and prolong the serum half-life of phenytoin by inhibiting its metabolism.
Chemistry[edit]
Phenytoin, 5,5-diphenylimidazolidinedione is synthesized in two different ways. The first involves a base catalyzed addition of urea to benzil followed by a benzilic acid rearrangement (1,2 phenyl migration) to form the desired product. This is known as the Biltz Synthesis of phenytoin.[5]

The second method involves the reaction of benzophenone with potassium cyanide in the presence of ammonium carbonate, followed by the simultaneous cyclization of the resulting product (carboxyaminonitrile) and its rearrangement under the reaction conditions to form phenytoin.
- US patent 2409754, Hense HR, "Method for obtaining hydantoins", issued 1946-10-22, assigned to Parke Davis
In popular culture[edit]
Dilantin made an appearance in the 1962 novel One Flew Over the Cuckoo's Nest by Ken Kesey, both as an anticonvulsant and as a mechanism to control inmate behavior.
In the 2013 science fiction film Elysium, the protagonist (played by Matt Damon) takes Miporol, a fictional brand name for diphenylhydantoin, after having been exposed to a lethal dose of radiation.
References[edit]
- ^ McEvoy, GK (2004). "AHFS drug information 2004". American Society of Health-System Pharmacists: 2117–2120.
- ^ Rogawski MA, Löscher W. The neurobiology of antiepileptic drugs. Nat Rev Neurosci. 2004 Jul;5(7):553-564 PubMed PMID 15208697.
- ^ Balaji S (2004). "Medical Therapy for Sudden Death". Pediatric Clinics of North America. 51 (5): 1379–1387. doi:10.1016/j.pcl.2004.04.002. PMID 15331289.
- ^ essential pharmacology by KD Tripathi 6E pg:405
- ^ a b Biltz H (1908). "Über die Konstitution der Einwirkungsprodukte von substituierten Harnstoffen auf Benzil und über einige neue Methoden zur Darstellung der 5,5-Diphenyl-hydantoine" [Constitution of the Products of the Interaction of Substituted Carbamides on Benzil and Certain New Methods for the Preparation of 5,5-Diphenylhydantoin]. Chemische Berichte (in German). 41 (1): 1379–1393. doi:10.1002/cber.190804101255.
- ^ Goodman and Gilman's Pharmacological Basis of Therapeutics (10th ed.). New York: McGraw-Hill. 2001.
- ^ Dreyfus J (1998). A Remarkable Medicine Has Been Overlooked: Including an Autobiography and the Clinical Section of the Broad Range of Use of Phenytoin. Continuum International Publishing Group. ISBN 0-8264-1069-3.
- ^ . FDA http://www.fda.gov/Drugs/GuidanceComplianceRegulatoryInformation/Surveillance/AdverseDrugEffects/ucm085914.htm. Retrieved 18 April 2014.
{{cite web}}: Missing or empty|title=(help) - ^ lippincots modern pharmacology with clinical applications pg no:377 5th Edition
- ^ "FDA drug label" (PDF). FDA. Retrieved 18 April 2014.
- ^ Clinical Pharmacology & Therapeutics 66, 563-568 (December 1999) | doi:10.1053/cp.1999.v66.103277001 Article Tools Send to a friend Export citation Rights and permissions Order commercial reprints Bookmark in Connotea Search Pubmed for Stephen Donahue David A. Flockhart Darrell R. Abernethy Ticlopidine inhibits phenytoin clearance*Ticlopidine inhibits phenytoin clearance *Supported in part by grants AG-08226-07 and GM-08386-08 from the National Institutes of Health, Bethesda, Md.
- ^ http://ebooks.cambridge.org/chapter.jsf?bid=CBO9781139103992&cid=CBO9781139103992A081
- ^ Chapter 67 - Antiepileptic drug pharmacokinetics and therapeutic drug monitoring pp. 358-366 By Philip N. Patsalos View chapter as PDF Antiepileptic drug pharmacokinetics and therapeutic drug monitoring By Philip N. Patsalos
- ^ http://www.mayomedicallaboratories.com/test-catalog/Clinical+and+Interpretive/9993
- ^ Pharmacology and pharmacotheraputics 22ed edition pg:129 By R S Satoskar
- ^ Shaw, J (2007 Nov). "The clinical effect of topical phenytoin on wound healing: a systematic review". The British Journal of Dermatology. 157 (5): 997–1004. doi:10.1111/j.1365-2133.2007.08160.x. PMID 17854378. S2CID 23862219.
{{cite journal}}: Check date values in:|date=(help); Unknown parameter|coauthors=ignored (|author=suggested) (help) - ^ Prathvi, Shetty (2013). "A Comparative Study of Efficacy of Topical Phenytoin vs Conventional Wound Care in Diabetic Ulcers". International Journal of Molecular Medical Science. doi:10.5376/ijmms.2013.03.0008.
- ^ Anstead, GM (1996 Jul-Aug). "Phenytoin in wound healing". The Annals of Pharmacotherapy. 30 (7–8): 768–75. doi:10.1177/106002809603000712. PMID 8826558. S2CID 20242305.
{{cite journal}}: Check date values in:|date=(help); Unknown parameter|coauthors=ignored (|author=suggested) (help) - ^ Bhatia, A (2004 Jul 15). "Topical phenytoin for wound healing". Dermatology Online Journal. 10 (1): 5. PMID 15347487.
{{cite journal}}: Check date values in:|date=(help); Unknown parameter|coauthors=ignored (|author=suggested) (help) - ^ Sinha SN & Amarasena I (FEBRUARY 2008). "Does phenytoin have a role in the treatment of pressure ulcers?". Wound Practice and Research. 16 (1): 37–41.
{{cite journal}}: Check date values in:|date=(help) - ^ Carl GF, Smith ML (1992). "Phenytoin-folate interactions: differing effects of the sodium salt and the free acid of phenytoin". Epilepsia. 33 (2): 372–375. doi:10.1111/j.1528-1157.1992.tb02330.x. PMID 1547769. S2CID 40927589.
- ^ http://www.netdoctor.co.uk/diseases/facts/aplasticanaemia.htm
- ^ Beckmann CR; et al. (2002). Obstetrics and Gynecology (4th ed.). Baltimore: Lippincott Williams & Wilkins.
{{cite book}}: Explicit use of et al. in:|author=(help) - ^ CDC. (2004). Fetal Alcohol Syndrome: Guidelines for Referral and Diagnosis. Can be downloaded at http://www.cdc.gov/fas/faspub.htm.
- ^ Adab N, Tudur SC, Vinten J, Williamson P, Winterbottom J (2004). Adab, Naghme (ed.). "Common Antiepileptic Drugs in Pregnancy in Women with Epilepsy". Cochrane Database of Systematic Reviews. 2004 (3): CD004848. doi:10.1002/14651858.CD004848. PMID 15266543.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - ^ Report on Carcinogens, Eleventh Edition (PB2005-104914, 2004) p III-216.
- ^ Maeda T, Sano N, Togei K, Shibata M, Izumi K, Otsuka H (1988). "Lack of carcinogenicity of phenytoin in (C57BL/6 x C3H)F1 mice". Journal of Toxicology and Environmental Health. 24 (1): 111–119. doi:10.1080/15287398809531144. PMID 3373561.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - ^ Arya R, Gulati S, Kabra M, Sahu JK, Kalra V (2011). "Folic acid supplementation prevents phenytoin-induced gingival overgrowth in children". Neurology. 76 (15): 1338–1343. doi:10.1212/WNL.0b013e3182152844. PMC 3090066. PMID 21482950.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - ^ FDA warns of risks from epilepsy drugs.
- ^ Scheinfeld N (2003). "Phenytoin in Cutaneous Medicine: Its Uses, Mechanisms and Side Effects". Dermatology Online Journal. 9 (3): 6. PMID 12952753.
- ^ a b Man CB, Kwan P, Baum L; et al. (2007). "Association between HLA-B*1502 allele and antiepileptic drug-induced cutaneous reactions in Han Chinese". Epilepsia. 48 (5): 1015–1018. doi:10.1111/j.1528-1167.2007.01022.x. PMID 17509004. S2CID 34728720.
{{cite journal}}: Explicit use of et al. in:|author=(help)CS1 maint: multiple names: authors list (link) Cite error: The named reference "pmid17509004" was defined multiple times with different content (see the help page). - ^ Carter, B. L.; Garnett, W. R.; Pellock, J. M.; Stratton, M. A.; Howell, J. R. (1981). "Effect of antacids on phenytoin bioavailability". Therapeutic Drug Monitoring. 3 (4): 333–40. doi:10.1097/00007691-198104000-00003. PMID 7336470. S2CID 26099092.
External links[edit]
- Medicines for Epilepsy: Dilantin Epilepsy Foundation.
- Remarkable Medicine, a website about the Dreyfus Foundation's work to expand the indications for phenytoin
- Phenytoin Pharmacokinetics (not a public link)
- [1] English Translation of 1908 German article on phenytoin synthesis by Heinrich Biltz
Category:Antiarrhythmic agents Category:Anticonvulsants Category:Hydantoins Category:Teratogens Category:World Health Organization essential medicines Category:IARC Group 2B carcinogens

