User:CFCF/sandbox/Lungs
| Lung | |
|---|---|
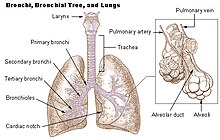
 Diagram showing the lungs, their fissures and lobes, the trachea, main and lobular bronchii, terminating in bronchioles. | |
 Subsection of a bronchiole showing alveoli and various relating structures | |
| Details | |
| System | Respiratory system |
| Identifiers | |
| Latin | pulmo |
| Greek | pneumo (πνεύμων) |
| Anatomical terminology | |
A major organ of the respiratory system, each lung houses structures of both the conducting and respiratory zones. The main function of the lungs is to perform the exchange of oxygen and carbon dioxide with air from the atmosphere. To this end, the lungs exchange respiratory gases across a very large epithelial surface area—about 70 square meters—that is highly permeable to gases.[1]
The human lungs are the organs of respiration. Humans have two lungs, a right lung and a left lung. The right lung consists of three lobes while the left lung is slightly smaller consisting of only two lobes (the left lung has a "cardiac notch" allowing space for the heart within the chest).[2] Together, the lungs contain approximately 2,400 kilometres (1,500 mi) of airways and 300 to 500 million alveoli.
Estimates of the total surface area of lungs vary from 30-50 square metres up to 70-100 square metres (1076.39 sq ft) (8,4 x 8,4 m) in adults — which might be roughly the same area as one side of a tennis court.[3] However, such estimates may be of limited use unless qualified by a statement of scale at which they are taken (see Coastline paradox and Menger sponge).
Furthermore, if all of the capillaries that surround the alveoli were unwound and laid end to end, they would extend for about 992 kilometres (616 mi). The lungs together weigh approximately 1.3 kilograms (2.9 lb), with the right lung weighing more than the left.
The pleural cavity is the potential space between the two serous membranes, (pleurae) of the lungs; the parietal pleura, lining the inner wall of the thoracic cage, and the visceral pleura, lining the organs themselves–the lungs. The respiratory system includes the conducting zone, which is part of the respiratory tract, that conducts air into the lungs.
The parenchyma of the lung, only relates to the functional alveolar tissue, but the term is often used to refer to all lung tissue, including the respiratory bronchioles, alveolar ducts, terminal bronchioles, and all connecting tissues.[4]
The lung is the essential respiration organ in many air-breathing animals, including most tetrapods, a few fish and a few snails. In mammals and the more complex life forms, the two lungs are located near the backbone on either side of the heart. Their principal function is to transport oxygen from the atmosphere into the bloodstream, and to release carbon dioxide from the bloodstream into the atmosphere. A large surface area is needed for this exchange of gases which is accomplished by the mosaic of specialized cells that form millions of tiny, exceptionally thin-walled air sacs called alveoli.
To understand the anatomy of the lungs, the passage of air through the nose and mouth to the alveoli must be studied. The progression of air through either the mouth or the nose, travels through the nasopharynx, oropharynx, larynx, and the trachea (windpipe). The air passes down the trachea, which divides into two main bronchi; these branch to the left and right lungs where they progressively subdivide into a system of bronchi and bronchioles until the alveoli are reached. These many alveoli are where the gas exchange of carbon dioxide and oxygen takes place.[5]
Breathing is driven by muscular action; in early tetrapods, air was driven into the lungs by the pharyngeal muscles via buccal pumping, which is still found in amphibians. Reptiles, birds and mammals use their musculoskeletal system to support and foster breathing.
Medical terms related to the lung often begin with pulmo-, such as in the (adjectival form: pulmonary) or from the Latin pulmonarius ("of the lungs"), or with pneumo- (from Greek πνεύμων "lung").
Structure[edit]
Gross anatomy[edit]
The lungs are pyramid-shaped, paired organs that are connected to the trachea by the right and left bronchi; on the inferior surface, the lungs are bordered by the diaphragm. The diaphragm is the flat, dome-shaped muscle located at the base of the lungs and thoracic cavity. The lungs are enclosed by the pleurae, which are attached to the mediastinum. The right lung is shorter and wider than the left lung, and the left lung occupies a smaller volume than the right. The cardiac notch is an indentation on the surface of the left lung, and it allows space for the heart (Figure). The apex of the lung is the superior region, whereas the base is the opposite region near the diaphragm. The costal surface of the lung borders the ribs. The mediastinal surface faces the midline.[1]

Each lung is composed of smaller units called lobes. Fissures separate these lobes from each other. The right lung consists of three lobes: the superior, middle, and inferior lobes. The left lung consists of two lobes: the superior and inferior lobes. A bronchopulmonary segment is a division of a lobe, and each lobe houses multiple bronchopulmonary segments. Each segment receives air from its own tertiary bronchus and is supplied with blood by its own artery. Some diseases of the lungs typically affect one or more bronchopulmonary segments, and in some cases, the diseased segments can be surgically removed with little influence on neighboring segments. A pulmonary lobule is a subdivision formed as the bronchi branch into bronchioles. Each lobule receives its own large bronchiole that has multiple branches. An interlobular septum is a wall, composed of connective tissue, which separates lobules from one another.[1]
Blood and nerve supply[edit]
The blood supply of the lungs plays an important role in gas exchange and serves as a transport system for gases throughout the body. In addition, innervation by the both the parasympathetic and sympathetic nervous systems provides an important level of control through dilation and constriction of the airway.[1]
Blood supply[edit]
The major function of the lungs is to perform gas exchange, which requires blood from the pulmonary circulation. This blood supply contains deoxygenated blood and travels to the lungs where erythrocytes, also known as red blood cells, pick up oxygen to be transported to tissues throughout the body. The pulmonary artery is an artery that arises from the pulmonary trunk and carries deoxygenated, arterial blood to the alveoli. The pulmonary artery branches multiple times as it follows the bronchi, and each branch becomes progressively smaller in diameter. One arteriole and an accompanying venule supply and drain one pulmonary lobule. As they near the alveoli, the pulmonary arteries become the pulmonary capillary network. The pulmonary capillary network consists of tiny vessels with very thin walls that lack smooth muscle fibers. The capillaries branch and follow the bronchioles and structure of the alveoli. It is at this point that the capillary wall meets the alveolar wall, creating the respiratory membrane. Once the blood is oxygenated, it drains from the alveoli by way of multiple pulmonary veins, which exit the lungs through the hilum.[1]
Nervous innervation[edit]
Dilation and constriction of the airway are achieved through nervous control by the parasympathetic and sympathetic nervous systems. The parasympathetic system causes bronchoconstriction, whereas the sympathetic nervous system stimulates bronchodilation. Reflexes such as coughing, and the ability of the lungs to regulate oxygen and carbon dioxide levels, also result from this autonomic nervous system control. Sensory nerve fibers arise from the vagus nerve, and from the second to fifth thoracic ganglia. The pulmonary plexus is a region on the lung root formed by the entrance of the nerves at the hilum. The nerves then follow the bronchi in the lungs and branch to innervate muscle fibers, glands, and blood vessels.[1]
Pleura[edit]

Each lung is enclosed within a cavity that is surrounded by the pleura. The pleura (plural = pleurae) is a serous membrane that surrounds the lung. The right and left pleurae, which enclose the right and left lungs, respectively, are separated by the mediastinum. The pleurae consist of two layers. The visceral pleura is the layer that is superficial to the lungs, and extends into and lines the lung fissures (Figure). In contrast, the parietal pleura is the outer layer that connects to the thoracic wall, the mediastinum, and the diaphragm. The visceral and parietal pleurae connect to each other at the hilum. The pleural cavity is the space between the visceral and parietal layers.[1]
Physiology[edit]
The physiology (or function) o

Respiration[edit]

The respiratory system's alveoli are the sites of gas exchange with blood.
- The sympathetic nervous system via noradrenaline acting on the beta receptors causes bronchodilation.
- The parasympathetic nervous system is through the vagus nerve,[6] via acetylcholine, which acts on the M-3 muscarinic receptors, maintains the resting tone of the bronchiolar smooth muscle. This action is related, although considered distinct from bronchoconstriction.
- Many other non-autonomic nervous and biochemical stimuli, including carbon dioxide and oxygen, are also involved in the regulation process.
There is also a relationship noted between the pressures in the lung, in the alveoli, in the arteries and in the veins. This is conceptualised into the lung being divided into three vertical regions called the zones of the lung.[7]
Respiratory system[edit]
The trachea divides at a junction–the carina of trachea, to give a right bronchus and a left bronchus, and this is usually at the level of the fifth thoracic vertebra. The conducting zone contains the trachea, the bronchi, the bronchioles, and the terminal bronchioles.
The respiratory system contains the respiratory bronchioles, the alveolar ducts, and the alveoli.
The conducting zone and the respiratory components, except the alveoli, comprise the air passageways, with gas exchange only taking place in the alveoli of the respiratory system. The conducting zone is reinforced with cartilage in order to hold open the airways. Air is warmed to 37 °C (99 °F), humidified and cleansed by the conduction zone; particles from the air being removed by the cilia which are located on the walls of all the passageways. The lungs are surrounded and protected by the rib cage.
Modification of substances[edit]
The lungs convert angiotensin I to angiotensin II. In addition, they remove several blood-borne substances, such as a few types of prostaglandins, leukotrienes, serotonin and bradykinin.[8]
Taste[edit]
In 2010, researchers found bitter taste receptors in lung tissue, which cause airways to relax when a bitter substance is encountered. They believe this mechanism is evolutionarily adaptive because it helps clear lung infections, but could also be exploited to treat asthma and chronic obstructive pulmonary disease.[9]
Non respiratory functions[edit]
In addition to their function in respiration, the lungs also:
- Alter the pH of blood by facilitating alterations in the partial pressure of carbon dioxide
- Filter out small blood clots formed in veins
- Filter out gas micro-bubbles occurring in the venous blood stream such as those created during decompression after underwater diving.[10]
- Influence the concentration of some biologic substances and drugs used in medicine in blood
- Convert angiotensin I to angiotensin II by the action of angiotensin-converting enzyme
- May serve as a layer of soft, shock-absorbent protection for the heart, which the lungs flank and nearly enclose.
- Immunoglobulin-A is secreted in the bronchial secretion and protects against respiratory infections.
- Maintain sterility by producing mucus containing antimicrobial compounds.[11] Mucus contains glycoproteins, e.g., mucins, lactoferrin,[12] lysozyme, lactoperoxidase.[13][14] We find also on the epithelium Dual oxidase 2[15][16][17] proteins generating hydrogen peroxide, useful for hypothiocyanite endogenous antimicrobial synthesis. Function not in place in cystic fibrosis patient lungs.[18][19]
- Ciliary escalator action is an important defence system against air-borne infection. The dust particles and bacteria in the inhaled air are caught in the mucous layer present at the mucosal surface of respiratory passages and are moved up towards pharynx by the rhythmic upward beating action of the cilia.
- Provide airflow for the creation of vocal sounds.
- The lungs serve as a reservoir of blood in the body. The blood volume of the lungs is about 450 milliliters on average, about 9 percent of the total blood volume of the entire circulatory system. This quantity can easily fluctuate from between one-half and twice the normal volume. Loss of blood from the systemic circulation by hemorrhage can be partially compensated for by shunting blood from the lungs into the systemic vessels[20]
- Thermoregulation via panting (observed in some animals, but not humans)
Clinical significance[edit]
The lungs are prone to infectious diseases. Tuberculosis is a serious infectious disease of the lung as is bacterial pneumonia.
Pulmonary fibrosis is a condition that can prove fatal. The lung tissue is replaced by fibrous connective tissue which causes irreversible lung scarring.
Lung cancer can often be incurable. Also cancers in other parts of the body can be spread via the bloodstream and end up in the lungs where the malignant cells can metastasise.
A pulmonary embolism is a blood clot that becomes lodged in the lung.
Development[edit]

The development of the human lungs arise from the laryngotracheal groove and develop to maturity over several weeks inside the foetus and for several months following birth.[21] The larynx, trachea, bronchi and lungs begin to form during the fourth week of embryogenesis.[22] At this time, the lung bud appears ventrally to the caudal portion of the foregut. The location of the lung bud along the gut tube is directed by various signals from the surrounding mesenchyme, including fibroblast growth factors. At the same time as the lung bud grows, the future trachea separates from the foregut through the formation of tracheoesophageal ridges, which fuse to form the tracheoesophageal septum.
The lung bud divides into two, the right and left primary bronchial buds.[23] During the fifth week the right bud branches into three secondary bronchial buds and the left branches into two secondary bronchial buds. These give rise to the lobes of the lungs, three on the right and two on the left. Over the following week the secondary buds branch into tertiary buds, about ten on each side.[24] From the sixth week to the sixteenth week, the major elements of the lungs appear except the alveoli, which makes survival, if born, impossible.[25] From week 16 to week 26, the bronchi enlarge and lung tissue becomes highly vascularised. Bronchioles and alveolar ducts also develop. During the period covering the 26th week until birth the important blood-air barrier is established. Specialised alveolar cells where gas exchange will take place, together with the alveolar cells that secrete pulmonary surfactant appear. The surfactant reduces the surface tension at the air-alveolar surface which allows expansion of the terminal saccules. These saccules form at the end of the bronchioles and their appearance marks the point at which limited respiration would be possible.[26]
First breath[edit]
At birth, the baby's lungs are filled with fluid secreted by the lungs and are not inflated. When the newborn is expelled from the birth canal, its central nervous system reacts to the sudden change in temperature and environment. This triggers it to take the first breath, within about 10 seconds after delivery.[27] The newborn lung is far from being a miniaturized version of the adult lung. It has only about 20,000,000 to 50,000,000 alveoli or 6 to 15 percent of the full adult compliment. Although it was previously thought that alveolar formation could continue to the age of eight years and beyond, it is now accepted that the bulk of alveolar formation is concluded much earlier, probably before the age of two years. The newly formed inter alveolar septa still contain a double capillary network instead of the single one of the adult lungs. This means that the pulmonary capillary bed must be completely reorganized during and after alveolar formation, it has to mature. Only after full microvascular maturation, which is terminated sometime between the ages of two and five years, is the lung development completed and the lung can enter a phase of normal growth.[28]
Other animals[edit]
Mammalian lungs[edit]
The lungs of mammals including those of humans, have a soft, spongelike texture and are honeycombed with epithelium, having a much larger surface area in total than the outer surface area of the lung itself.
Breathing is largely driven by the muscular diaphragm at the bottom of the thorax. Contraction of the diaphragm pulls the bottom of the cavity in which the lung is enclosed downward, increasing volume and thus decreasing pressure, causing air to flow into the airways. Air enters through the oral and nasal cavities; it flows through the pharynx, then the larynx and into the trachea, which branches out into the main bronchi and then subsequent divisions. During normal breathing, expiration is passive and no muscles are contracted (the diaphragm relaxes). The rib cage itself is also able to expand and contract to some degree through the use of the intercostal muscles, together with the action of other respiratory and accessory respiratory muscles. As a result, air is transported into or expelled out of the lungs. This type of lung is known as a bellows lung as it resembles a blacksmith's bellows.[29]
Anatomy[edit]
In humans, the trachea divides into the two main bronchi that enter the roots of the lungs. The bronchi continue to divide within the lung, and after multiple divisions, give rise to bronchioles. The bronchial tree continues branching until it reaches the level of terminal bronchioles, which lead to alveolar sacs. Alveolar sacs, are made up of clusters of alveoli, like individual grapes within a bunch. The individual alveoli are tightly wrapped in blood vessels and it is here that gas exchange actually occurs. Deoxygenated blood from the heart is pumped through the pulmonary artery to the lungs, where oxygen diffuses into blood and is exchanged for carbon dioxide in the haemoglobin of the erythrocytes. The oxygen-rich blood returns to the heart via the pulmonary veins to be pumped back into systemic circulation."Lung Disease & Respiratory Health Center".
Human lungs are located in two cavities on either side of the heart. Though similar in appearance, the two are not identical. Both are separated into lobes by fissures, with three lobes on the right and two on the left. The lobes are further divided into segments and then into lobules, hexagonal divisions of the lungs that are the smallest subdivision visible to the naked eye.[citation needed] The connective tissue that divides lobules is often blackened in smokers. The medial border of the right lung is nearly vertical, while the left lung contains a cardiac notch. The cardiac notch is a concave impression molded to accommodate the shape of the heart.
Each lobe is surrounded by a pleural cavity, which consists of two pleurae. The parietal pleura lies against the rib cage, and the visceral pleura lies on the surface of the lungs. In between the pleura is pleural fluid. The pleural cavity helps to lubricate the lungs, as well as providing surface tension to keep the lung surface in contact with the rib cage.
Lungs are to a certain extent 'overbuilt' and have a tremendous reserve volume as compared to the oxygen exchange requirements when at rest. Such excess capacity is one of the reasons that individuals can smoke for years without having a noticeable decrease in lung function while still or moving slowly; in situations like these only a small portion of the lungs are actually perfused with blood for gas exchange. Destruction of too many alveoli over time leads to the condition emphysema, which is associated with extreme shortness of breath. As oxygen requirements increase due to exercise, a greater volume of the lungs is perfused, allowing the body to match its CO2/O2 exchange requirements. Additionally, due to the excess capacity, it is possible for humans to live with only one lung, with the one compensating for the other's loss.
The environment of the lung is very moist, which makes it hospitable for bacteria. Many respiratory illnesses are the result of bacterial or viral infection of the lungs. Inflammation of the lungs is known as pneumonia; inflammation of the pleura surrounding the lungs is known as pleurisy.
Vital capacity is the maximum volume of air that a person can exhale after maximum inhalation; it can be measured with a spirometer. In combination with other physiological measurements, the vital capacity can help make a diagnosis of underlying lung disease.
The lung parenchyma is strictly used to refer solely to alveolar tissue with respiratory bronchioles, alveolar ducts and terminal bronchioles.[4] However, it often includes any form of lung tissue, also including bronchioles, bronchi, blood vessels and lung interstitium.[4]
Avian lungs[edit]


Avian lungs do not have alveoli as mammalian lungs do; birds have honey-comb-like, faveolar lungs, which contain millions of tiny passages called parabronchi. There are air vesicles, called atria, which project radially from the walls of the parabronchi. The gas exchange tissues are set into the walls of the atria and gases travel via diffusion between the gas exchange tissues and the lumen of each parabronchus. There are two categories of parabronchi. The paleopulmonic parabronchi are found in all birds and air flows through them in the same direction—posterior to anterior during inhalation and exhalation. Some bird species also have neopulmonic parabronchi where the air flow is bidirectional. The paleopulmonic unidirectional airflow is in contrast to the mammalian system, in which the direction of airflow in the lung is tidal, reversing between inhalation and exhalation.
By utilizing a unidirectional flow of air, avian lungs are able to extract a greater concentration of oxygen from inhaled air. Birds are thus equipped to fly at altitudes at which mammals would succumb to hypoxia. This also allows them to sustain a higher metabolic rate than most equivalent weight mammals.[30] Note than some species of small bats have a higher mean total morphometric pulmonary diffusing capacity for oxygen than equivalent weight birds but this is the exception and is not the rule.[31]
The lungs of birds are relatively small, but are connected to 8–9 air sacs that extend through much of the body, and are in turn connected to air spaces within the bones. The air sacs, although thin walled, are poorly vascularized, and do not themselves contribute much to gas exchange, but they do act like bellows to ventilate the lungs. The air sacs expand and contract due to changes in the volume of the combined thorax and abdominal cavity. This volume change is caused by the movement of the sternum and ribs and this movement is often synchronized with movement of the flight muscles.[32]
Because of the complexity of the system, misunderstanding is common and it is incorrectly believed that it takes two breathing cycles for air to pass entirely through a bird's respiratory system. Air is not stored in either the posterior or anterior sacs between respiration cycles, air moves continuously from the posterior to the anterior of the lungs throughout respiration. This type of lung construction is called a circulatory lung, as distinct from the bellows lung possessed by other animals.[30]
Reptilian lungs[edit]
Reptilian lungs are typically ventilated by a combination of expansion and contraction of the ribs via axial muscles and buccal pumping. Crocodilians also rely on the hepatic piston method, in which the liver is pulled back by a muscle anchored to the pubic bone (part of the pelvis), which in turn pulls the bottom of the lungs backward, expanding them. Turtles, which are unable to move their ribs, instead use their forelimbs and pectoral girdle to force air in and out of the lungs.[32]
The lung of most reptiles has a single bronchus running down the centre, from which numerous branches reach out to individual pockets throughout the lungs. These pockets are similar to, but much larger and fewer in number than, mammalian alveoli, and give the lung a sponge-like texture. In tuataras, snakes, and some lizards, the lungs are simpler in structure, similar to that of typical amphibians.[32]
Snakes and limbless lizards typically possess only the right lung as a major respiratory organ; the left lung is greatly reduced, or even absent. Amphisbaenians, however, have the opposite arrangement, with a major left lung, and a reduced or absent right lung.[32]
Both crocodilians and monitor lizards have developed lungs similar to those of birds, providing an unidirectional airflow and even possessing air sacs.[33] The now extinct pterosaurs have seemingly even further refined this type of lung, extending the airsacs into the wing membranes and, in the case of Pteranodontia, the hindlimbs.
Amphibian lungs[edit]
The lungs of most frogs and other amphibians are simple balloon-like structures, with gas exchange limited to the outer surface area of the lung. This is not a very efficient arrangement, but amphibians have low metabolic demands and can also quickly dispose of carbon dioxide by diffusion across their skin in water, and supplement their oxygen supply by the same method. Unlike higher vertebrates, who use a breathing system driven by negative pressure where the lungs are inflated by expanding the rib cage, amphibians employ positive pressure system, forcing air down into the lungs by buccal pumping.[34] The floor of the mouth is lowered, filling the mouth cavity with air. The throat muscles then presses the throat against the underside of the skull, forcing the air into the lungs.[35]
Due to the possibility of respiration across the skin combined with small size, all known lungless tetrapods are amphibians. The majority of salamander species are lungless salamanders, which respirate through their skin and tissues lining their mouth. This necessarily restrict their size, all are small and rather thread-like in appearance, maximizing skin surface relative to body volume.[36] The only other known lungless tetrapods are the Bornean Flat-headed Frog (Barbourula kalimantanensis) and Atretochoana eiselti, a caecilian.
The lungs of amphibians typically have a few narrow septa of soft tissue around the outer walls, increasing the respiratory surface area and giving the lung a honey-comb appearance. In some salamanders even these are lacking, and the lung has a smooth wall. In caecilians, as in snakes, only the right lung attains any size or development.[32]
Lungfish[edit]
The lungs of lungfish are similar to those of amphibians, with few, if any, internal septa. In the Australian lungfish, there is only a single lung, albeit divided into two lobes. Other lungfish and Polypterus, however, have two lungs, which are located in the upper part of the body, with the connecting duct curving round and above the esophagus. The blood supply also twists around the esophagus, suggesting that the lungs originally evolved in the ventral part of the body, as in other vertebrates.[32]
Invertebrate lungs[edit]
Some invertebrates have "lungs" that serve a similar respiratory purpose as, but are not evolutionarily related to, vertebrate lungs. Some arachnids have structures called "book lungs" used for atmospheric gas exchange. The Coconut crab uses structures called Branchiostegal lungs to breathe air and indeed will drown in water, hence it breathes on land and holds its breath underwater. The Pulmonata are an order of snails and slugs that have developed "lungs".
Origins of the vertebrate lung[edit]
The lungs of today's terrestrial vertebrates and the gas bladders of today's fish are believed to have evolved from simple sacs (outpocketings) of the esophagus that allowed early fish to gulp air under oxygen-poor conditions.[37] These outpocketings first arose in the bony fish. In most of the ray-finned fish the sacs evolved into closed off gas bladders, while a number of carps, trouts, herrings, catfish, eels has retained the physostome condition with the sack being open to the esophagus. In more basal bony fish, such as the gar, bichir, bowfin and the lobe-finned fish, the bladders have evolved to primarily function as lungs.[37] The lobe-finned fish gave rise to the land-based tetrapods. Thus, the lungs of vertebrates are homologous to the gas bladders of fish (but not to their gills). This is reflected by the fact that the lungs of a fetus also develop from an outpocketing of the esophagus and in the case of the physostome gas bladders, which can serve as both buoyancy organ and with the pneumatic duct to the gut also serve as lungs. This condition is found in more "primitive" teleosts, and is lost in the higher orders. (This is an instance of correlation between ontogeny and phylogeny.) No known animals have both a gas bladder and lungs.
Structure[edit]
The lungs are located within the thoracic cavity, on either side of the heart and close to the backbone. They are enclosed and protected by the ribcage. The left lung has a lateral indentation which is shaped to accommodate the position of the heart. The right lobe is a little shorter than the left lung and this is to accommodate the positioning of the liver. Both lungs have broad bases enabling them to rest on the diaphragm without causing displacement. Each lung near to the centre has a recessed region called the hilum which is the entry point for the root of the lung. (Root here means the anchoring part of a structure.) The bronchi and pulmonary vessels extend from the heart and the trachea to connect each lung by way of the root.
There are three surfaces to the lungs: the costal surface is the outer, thoracic surface which is smooth and convex. This surface area is large and corresponds to the form of the thoracic cavity, being deeper at the back than at the front. The costal surface is in contact with the costal pleura and in specimens that have been hardened in situ, slight grooves are visible which correspond to the overlying ribs.The mediastinal surface of the lung is in contact with the mediastinal pleura and presents the cardiac impression. The diaphragmatic surface of lung is the portion of the lung which borders on the thoracic diaphragm.
Right lung[edit]

The right lung is divided into three lobes (as opposed to two lobes on the left), superior, middle, and inferior, by two interlobular fissures:
The right lung has a higher volume, total capacity and weight, than that of the left lung. Although it is 5 cm shorter due to the diaphragm rising higher on the right side to accommodate the liver, it is broader than the left lung due to the cardiac notch of the left lung.
- Fissures
- The lower, oblique fissure, separates the inferior from the middle and superior lobes, and is closely aligned with the fissure in the left lung. Its direction is, however, more vertical, and it cuts the lower border about 7.5 cm. behind its anterior extremity.
- The upper, horizontal fissure, separates the superior from the middle lobe. It begins in the lower fissure near the posterior border of the lung, and, running horizontally forward, cuts the anterior border on a level with the sternal end of the fourth costal cartilage; on the mediastinal surface it may be traced backward to the hilum.
- Lobes
The middle lobe is the smallest lobe of the right lung. It is wedge-shaped, and includes the part of the anterior border, and the anterior part of the base of the lung. The superior and inferior lobes are similar to those of the left lung (which lacks a middle lobe.)
- Impressions
There is a deep concavity on the mediastinal surface called the cardiac impression, which accommodates the pericardium; this is not as pronounced as that on the left lung where the heart projects further. On the same surface, immediately above the hilum, is an arched furrow which accommodates the azygos vein; while running superiorly, and then arching laterally some little distance below the apex, is a wide groove for the superior vena cava and right innominate vein; behind this, and proximal to the apex, is a furrow for the innominate artery.
Behind the hilum and the attachment of the pulmonary ligament is a vertical groove for the esophagus; this groove becomes less distinct below, owing to the inclination of the lower part of the esophagus to the left of the middle line.
In front and to the right of the lower part of the esophageal groove is a deep concavity for the extrapericardiac portion of the thoracic part of the inferior vena cava.
Left lung[edit]

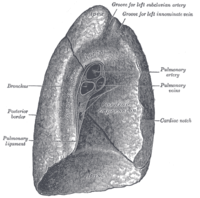
The left lung is divided into two lobes, an upper and a lower, by the oblique fissure, which extends from the costal to the mediastinal surface of the lung both above and below the hilum. The left lung, unlike the right does not have a middle lobe. However the term lingula is used to denote a projection of the upper lobe of the left lung that serves as the homologue. This area of the left lobe - the lingula, means little tongue (in Latin) and is often referred to as the tongue in the lung. There are two bronchopulmonary segments of the lingula: superior and inferior. It is thought that the lingula of the left lung is the remnant of the middle lobe, which has been lost through evolution.
- Surfaces
As seen on the surface, this fissure begins on the mediastinal surface of the lung at the upper and posterior part of the hilum, and runs backward and upward to the posterior border, which it crosses at a point about 6 cm. below the apex.
It then extends downward and forward over the costal surface, and reaches the lower border a little behind its anterior extremity, and its further course can be followed upward and backward across the mediastinal surface as far as the lower part of the hilum.
- Impressions
There is a large and deep concavity called the cardiac impression, on the mediastinal surface to accommodate the pericardium. On the same surface, immediately above the hilum, is a well-marked curved furrow produced by the aortic arch, and running upward from this toward the apex is a groove accommodating the left subclavian artery; a slight impression in front of the latter and close to the margin of the lung lodges the left innominate vein.
Behind the hilum and pulmonary ligament is a vertical furrow produced by the descending aorta, and in front of this, near the base of the lung, the lower part of the esophagus causes a shallow impression.
See also[edit]
- Alveolar-capillary barrier
- American Lung Association
- Asthma
- Borders of the lung
- Bronchitis
- Bronchus
- Cardiothoracic surgery
- Chronic obstructive pulmonary disease
- Drowning
- Dry drowning
- Emphysema
- Gills
- Left lung
- Liquid breathing
- Lung cancer
- Lung volumes
- Mechanical ventilation
- Pneumothorax
- Pneumonia
- Pulmonary contusion
- Pulmonology
- Right lung
- Tuberculosis
External links[edit]
- Lung Function Fundamentals, anaesthetist.com
- Dr D.R. Johnson: Introductory anatomy, respiratory system, leeds.ac.uk
- Franlink Institute Online: The Respiratory System, sln.fi.edu
- Chronic Respiratory Disease - leading research and articles on respiratory disease, crd.sagepub.com
- Avian lungs and respiration, people.eku.edu
Additional images[edit]
-
Left lung
-
Diagram of the respiratory system
-
Anatomy of lungs
-
Front view of heart and lungs
-
Transverse section of thorax, showing relations of pulmonary artery
-
The position and relation of the esophagus in the cervical region and in the posterior mediastinum, seen from behind
-
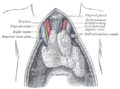
The thymus of a full-time fetus, exposed in situ
-
Sketch of the human lungs.
-
The human lungs flank the heart and great vessels in the chest cavity[38]
-
Air enters and leaves the lungs via a conduit of cartilaginous passageways—the bronchi and bronchioles. In this image, lung tissue has been dissected away to reveal the bronchioles[38]
- Dissection
-
Human right lung
-
Human embryo, 38 mm, 8–9 weeks.
References[edit]
![]() This article incorporates text in the public domain from the 20th edition of Gray's Anatomy (1918)
This article incorporates text in the public domain from the 20th edition of Gray's Anatomy (1918)
This article incorporates text from the CC BY book: OpenStax College, Anatomy & Physiology. OpenStax CNX. 30 July 2014.
- ^ a b c d e f g Betts, J. Gordon (2013). Anatomy & physiology. pp. 997–999. ISBN 1938168135. Retrieved 6 October 2014.
- ^ Tomco, Rachel. "Lungs and Mechanics of Breathing". AnatomyOne. Amirsys, Inc. Retrieved 2012-09-28.
- ^ Notter, Robert H. (2000). Lung surfactants: basic science and clinical applications. New York, N.Y: Marcel Dekker. p. 120. ISBN 0-8247-0401-0. Retrieved 2008-10-11.
- ^ a b c medilexicon.com > Medical Dictionary - 'Parenchyma Of Lung' In turn citing: Stedman's Medical Dictionary. 2006
- ^ Wienberger, Cockrill, Mandel. Principles of Pulmonary Medicine. Elsevier Science.[verification needed]
- ^ http://web.carteret.edu/keoughp/LFreshwater/PHARM/Blackboard/PNS/Neural%20Control%20of%20Lung%20Function.htm
- ^ Permutt S, Bromberger-Barnea B, Bane H.N (1962). "Alveolar Pressure, Pulmonary Venous Pressure, and the Vascular Waterfall". Med. thorac. 19: 239–269. doi:10.1159/000192224.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - ^ Walter F., PhD. Boron (2004). Medical Physiology: A Cellular And Molecular Approaoch. Elsevier/Saunders. ISBN 1-4160-2328-3. Page 605
- ^ Taste Receptors | University of Maryland Medical Center
- ^ Wienke B.R.: "Decompression theory"[verification needed]
- ^ Travis SM, Conway BA, Zabner J; et al. (May 1999). "Activity of abundant antimicrobials of the human airway". American Journal of Respiratory Cell and Molecular Biology. 20 (5): 872–9. doi:10.1165/ajrcmb.20.5.3572. PMID 10226057.
{{cite journal}}: Explicit use of et al. in:|author=(help)CS1 maint: multiple names: authors list (link) - ^ Rogan MP, Taggart CC, Greene CM, Murphy PG, O'Neill SJ, McElvaney NG (October 2004). "Loss of microbicidal activity and increased formation of biofilm due to decreased lactoferrin activity in patients with cystic fibrosis". The Journal of Infectious Diseases. 190 (7): 1245–53. doi:10.1086/423821. PMID 15346334.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - ^ Wijkstrom-Frei C, El-Chemaly S, Ali-Rachedi R; et al. (August 2003). "Lactoperoxidase and human airway host defense". American Journal of Respiratory Cell and Molecular Biology. 29 (2): 206–12. doi:10.1165/rcmb.2002-0152OC. PMID 12626341.
{{cite journal}}: Explicit use of et al. in:|author=(help)CS1 maint: multiple names: authors list (link) - ^ Conner GE, Salathe M, Forteza R (December 2002). "Lactoperoxidase and hydrogen peroxide metabolism in the airway". American Journal of Respiratory and Critical Care Medicine. 166 (12 Pt 2): S57–61. doi:10.1164/rccm.2206018. PMID 12471090.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - ^ Fischer H (October 2009). "Mechanisms and Function of DUOX in Epithelia of the Lung". Antioxidants & Redox Signaling. 11 (10): 2453–65. doi:10.1089/ARS.2009.2558. PMC 2823369. PMID 19358684.
- ^ Rada B, Leto TL (2008). "Oxidative innate immune defenses by Nox/Duox family NADPH Oxidases". Contributions to Microbiology. Contributions to Microbiology. 15: 164–87. doi:10.1159/000136357. ISBN 978-3-8055-8548-4. PMC 2776633. PMID 18511861.
- ^ Rada B, Lekstrom K, Damian S, Dupuy C, Leto TL (October 2008). "The Pseudomonas toxin pyocyanin inhibits the Dual oxidase-based antimicrobial system as it imposes oxidative stress on airway epithelial cells". Journal of Immunology. 181 (7): 4883–93. doi:10.4049/jimmunol.181.7.4883. PMC 2776642. PMID 18802092.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - ^ Moskwa P, Lorentzen D, Excoffon KJ; et al. (January 2007). "A Novel Host Defense System of Airways Is Defective in Cystic Fibrosis". American Journal of Respiratory and Critical Care Medicine. 175 (2): 174–83. doi:10.1164/rccm.200607-1029OC. PMC 2720149. PMID 17082494.
{{cite journal}}: Explicit use of et al. in:|author=(help)CS1 maint: multiple names: authors list (link) - ^ Conner GE, Wijkstrom-Frei C, Randell SH, Fernandez VE, Salathe M (January 2007). "The Lactoperoxidase System Links Anion Transport To Host Defense in Cystic Fibrosis". FEBS Letters. 581 (2): 271–8. doi:10.1016/j.febslet.2006.12.025. PMC 1851694. PMID 17204267.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - ^ GUYTON&HALL Medical physiology 12th edition
- ^ Sadler T (2003). Langman's Medical Embryology (9th ed. ed.). Lippincott Williams & Wilkins. ISBN 0-7817-4310-9.
{{cite book}}:|edition=has extra text (help) - ^ Moore KL, Persaud TVN (2002). The Developing Human: Clinically Oriented Embryology (7th ed. ed.). Saunders. ISBN 0-7216-9412-8.
{{cite book}}:|edition=has extra text (help) - ^ Larsen WJ. Human Embryology 2001.Page 144
- ^ Larsen WJ. Human Embryology 2001. Page 144
- ^ Kyung Won, PhD. Chung (2005). Gross Anatomy (Board Review). Hagerstown, MD: Lippincott Williams & Wilkins. p. 156. ISBN 0-7817-5309-0.
- ^ Dorlands Medical Dictionary 2012 Page 1660
- ^ About.com > Changes in the newborn at birth Review Date: 27 November 2007. Reviewed By: Deirdre OReilly, MD
- ^ Burri, P (n.d). lungdevelopment. Retrieved March 21, 2012, from www.briticannica.com/EBchecked/topic/499530/human-respiration/66137/lung-development
- ^ Maton, Anthea; Jean Hopkins; Charles William McLaughlin; Susan Johnson; Maryanna Quon Warner; David LaHart; Jill D. Wright1 (1993). Human Biology and Health. Englewood Cliffs, New Jersey, USA: Prentice Hall. ISBN 0-13-981176-1. OCLC 32308337.
{{cite book}}: CS1 maint: numeric names: authors list (link)[page needed] - ^ a b Ritchson, G. "BIO 554/754 - Ornithology: Avian respiration". Department of Biological Sciences, Eastern Kentucky University. Retrieved 2009-04-23.
- ^ Maina, John N.; A. S. King (July 1, 1984). "Correlations between structure and function in the design of the bat lung: a morphometric study" (PDF). Journal of Experimental Biology. 111 (1): 43–61. Retrieved 14 January 2012.
- ^ a b c d e f Romer, Alfred Sherwood; Parsons, Thomas S. (1977). The Vertebrate Body. Philadelphia, PA: Holt-Saunders International. pp. 330–334. ISBN 0-03-910284-X.
- ^ Unidirectional Airflow In The Lungs Of Birds, Crocs And Now Monitor Lizards
- ^ Janis, C.M.; Keller, J.C. (2001). "Modes of ventilation in early tetrapods: Costal aspiration as a key feature of amniotes" (PDF). Acta Palaeontologica Polonica. 46 (2): 137–170. Retrieved 11 May 2012.
- ^ Brainerd, E. L. (1999). New perspectives on the evolution of lung ventilation mechanisms in vertebrates. Experimental Biology Online 4, 11-28. http://www.brown.edu/Departments/EEB/brainerd_lab/pdf/Brainerd-1999-EBO.pdf
- ^ Duellman, W. E.; Trueb, L. (1994). Biology of amphibians. illustrated by L. Trueb. Johns Hopkins University Press. ISBN 0-8018-4780-X.
- ^ a b Colleen Farmer (1997). "Did lungs and the intracardiac shunt evolve to oxygenate the heart in vertebrates" (PDF). Paleobiology.
- ^ a b Gray's Anatomy of the Human Body, 20th ed. 1918.
Category:Lung Category:Human lung Category:Human anatomy by organ







![The human lungs flank the heart and great vessels in the chest cavity[38]](http://upload.wikimedia.org/wikipedia/commons/thumb/e/e6/Heart-and-lungs.jpg/120px-Heart-and-lungs.jpg)
![Air enters and leaves the lungs via a conduit of cartilaginous passageways—the bronchi and bronchioles. In this image, lung tissue has been dissected away to reveal the bronchioles[38]](http://upload.wikimedia.org/wikipedia/commons/thumb/7/7a/Gray962.png/120px-Gray962.png)

