User:Bozal243/sandbox
Article under construction for writing course. Planned on being completed by late April. Please don't delete. A bioartificial liver device (BAL) is an artificial extracorporeal supportive device for individuals suffering from acute liver failure. The device is extracorporeal because the process is performed outside of the body. They are considered bio-artificial because they are made up of manufactured and biological components.[1] BALs differ from artificial liver devices by incorporating synthetic functions alongside homeostasis. Synthetic functions include making necessary proteins for the body such as albumin and clotting factors. [2]
History[edit]
Early History[edit]
The first bioartificial liver device was developed by Dr. Kenneth Matsumara and was named an invention of the year by Time magazine in 2001.[3] Liver cells obtained from an animal were used instead of developing a piece of equipment for each function of the liver. The structure and function of the first device resembles that of todays BALs. Animal liver cells are suspended in a solution and a patients blood are separated by a semipermeable membrane that allow toxins and blood proteins to pass but restricts an immunological response.[3]
Development[edit]
Advancements in Biological engineering techniques in the decade after Matsumara's work have led to improved membrane constructs and hepatocyte attachment systems. [4] As time has progressed the sources of hepatocytes have increased. Cell sources now include primary porcine hepatocytes, primary human hepatocytes, human hepatoblastoma (C3A), immortalized human cell lines and stem cells.[4]
Use[edit]
The current purpose of BAL-type devices is not to permanently replace liver functions, but to serve as a supportive device. [5] BAL support allows the liver to regenerate properly upon acute liver failure, or serves to bridge the individual's liver functions until a transplant is possible.[4]
Function[edit]
BALs are essentially bioreactors with embedded hepatocytes (liver cells) that perform the functions of a normal liver. They process oxygenated blood plasma, which is separated from the other blood constituents.[6] Several types of BALs are being developed, including hollow fiber systems and flat membrane sheet systems.[7] A common bioreactor design incorporates the use of a membrane to prevent the direct contact of blood or plasma with the isolated hepatocytes. Some membranes have a molecular weight cutoff that restricts the movement of immunoglobulin, preventing immune-mediated injury. The cutoff, however, allows the transport of toxins from the blood and albumin from the hepatocytes. The advantages of using a BAL, over other dialysis-type devices (e.g. liver dialysis), is that metabolic functions (such as lipid and plasma lipoprotein synthesis, regulation of carbohydrate homeostasis, production of serum albumin and clotting factors, etc.), and detoxification. These processes can be replicated without the use of multiple devices.
Hollow fiber system[edit]
One type of BAL similar to kidney dialysis employs a hollow fiber cartridge system. Blood plasma is first separated from blood. In some devices the plasma passes through activated charcoal and an oxygenator before or after being run through hollow fibers. This serves as an initial detoxification step and improves oxygen delivery upstream. Hepatocytes from a variety of sources, such as porcine or human hepatoblastoma cell lines, are immobilized in a substrate outside of the fibers.[8] The semi-permeable hollow fibers allow for the transport of oxygen and nutrients from the blood to the hepatocytes. It isolates cells from the immune factors which are much larger. Toxins, metabolites and synthesized proteins, such as albumin and coagulation factors, are able to cross the membrane.
Extracorporeal liver assist device[edit]
The extracorporeal liver assist device (ELAD), developed by Vital Therapies[9], uses hollow-fiber technology with human hepatoblastoma cells. It is one of the few BAL devices undergoing clinical trials.[4]
HepatAssist[edit]
The HepatAssist device, developed by Circe Biomedical, uses hollow-fiber technology with porcine hepatocytes.[10] Also undergoing clinical trials, it has been shown that individuals with ALF have a survival advantage when treated with the device.[4]
Flat membrane sheet system[edit]
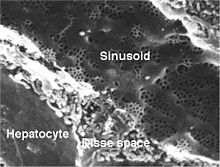
In the flat membrane sheet system hepatocytes are attached to a flat surface. The cells are attached as a monolayer in the effort of mimicing the liver sinusoid. Flow distribution is easily controlled in this system allowing for maximum contact between the hepatocytes and filtered blood plasma.[4] Drawbacks associated with this system include the difficulty in scale up and the high shear stress the cells are subject to. Attachment of hepatocytes to grooved surfaces has been shown to lessen their exposure to the deleterious effects of shear stress. [4]
Trials[edit]
A series of studies in 2004 showed that a BAL device reduced mortality by about half in acute liver failure cases.[11] The studies, which covered 171 patients in the U.S. and Europe, compared standard supportive care to the use of a bioreactor device using pig liver cells.
See also[edit]
References[edit]
- ^ https://www.alinfoundation.com/Medical%20Research/Liver.htm
- ^ http://iuhealth.org/riley/gastroenterology-hepatology-nutrition/liver-overview/how-the-liver-works/
- ^ a b http://content.time.com/time/specials/packages/article/0,28804,1936165_1936238_1936293,00.html
- ^ a b c d e f g Tilles A, Berthiaume F, Yarmush M, Tompkins R, Toner M (2002). "Bioengineering of liver assist devices". Hepatobiliary Pancreat Surg. 9 (6): 686–696. doi:10.1007/s005340200095. PMID 09441166.
{{cite journal}}: CS1 maint: multiple names: authors list (link) [1]. - ^ Allen J, Hassanein T, Bhatia S (2001). "Advances in bioartificial liver devices". Hepatology. 34 (3): 447–55. doi:10.1053/jhep.2001.26753. PMID 11526528.
{{cite journal}}: CS1 maint: multiple names: authors list (link) Free Full Text. - ^ Strain A, Neuberger J (2002). "A bioartificial liver--state of the art". Science. 295 (5557): 1005–9. doi:10.1126/science.1068660. PMID 11834813.
- ^ Current Work on the Bioartificial Liver
- ^ Carpentier B, Gautier A, Legallais C (2009). "Artificial and bioartificial liver devices: Present and future". Gut. 58 (12): 1690–1702. doi:10.1136/gut.2008.175380.
{{cite journal}}: CS1 maint: multiple names: authors list (link) [2]. - ^ http://vitaltherapies.com/elad/technology/
- ^ http://biomed.brown.edu/Courses/BI108/BI108_1999_Groups/Liver_Team/Liver.html#systemsin
- ^ Major study: Bioartificial liver reduces mortality by 44 percent in acute liver-failure patients
Category:Biological engineering
Category:Digestive system procedures
Category:Hepatology
Category:Medical equipment
Category:Medical treatments

