User:Zchas2/sandbox
Template:Good article is only for Wikipedia:Good articles.
| Zchas2/sandbox |
|---|
Syphilis is a sexually transmitted infection caused by the spirochete bacterium Treponema pallidum subspecies pallidum. The primary route of transmission is through sexual contact; it may also be transmitted from mother to fetus during pregnancy or at birth, resulting in congenital syphilis. Other human diseases caused by related Treponema pallidum include yaws (subspecies pertenue), pinta (subspecies carateum), and bejel (subspecies endemicum).
The signs and symptoms of syphilis vary depending in which of the four stages it presents (primary, secondary, latent, and tertiary). The primary stage classically presents with a single chancre (a firm, painless, non-itchy skin ulceration), secondary syphilis with a diffuse rash which frequently involves the palms of the hands and soles of the feet, latent syphilis with little to no symptoms, and tertiary syphilis with gummas, neurological, or cardiac symptoms. It has, however, been known as "the great imitator" due to its frequent atypical presentations. Diagnosis is usually via blood tests; however, the bacteria can also be detected using dark field microscopy. Syphilis can be effectively treated with antibiotics, specifically the preferred intramuscular penicillin G (given intravenously for neurosyphilis), or else ceftriaxone, and in those who have a severe penicillin allergy, oral doxycycline or azithromycin.
Syphilis is thought to have infected 12 million people worldwide in 1999, with greater than 90% of cases in the developing world. After decreasing dramatically since the widespread availability of penicillin in the 1940s, rates of infection have increased since the turn of the millennium in many countries, often in combination with human immunodeficiency virus (HIV). This has been attributed partly to unsafe sexual practices among men who have sex with men, increased promiscuity, prostitution, and decreasing use of condoms.[1][2][3]
Signs and symptoms[edit]
Syphilis can present in one of four different stages: primary, secondary, latent, and tertiary,[4] and may also occur congenitally.[5] It was referred to as "the great imitator" by Sir William Osler due to its varied presentations.[4][6]
Primary[edit]
Primary syphilis is typically acquired by direct sexual contact with the infectious lesions of another person.[7] Approximately 3 to 90 days after the initial exposure (average 21 days) a skin lesion, called a chancre, appears at the point of contact.[4] This is classically (40% of the time) a single, firm, painless, non-itchy skin ulceration with a clean base and sharp borders between 0.3 and 3.0 cm in size.[4] The lesion, however, may take on almost any form.[8] In the classic form, it evolves from a macule to a papule and finally to an erosion or ulcer.[8] Occasionally, multiple lesions may be present (~40%),[4] with multiple lesions more common when coinfected with HIV. Lesions may be painful or tender (30%), and they may occur outside of the genitals (2–7%). The most common location in women is the cervix (44%), the penis in heterosexual men (99%), and anally and rectally relatively commonly in men who have sex with men (34%).[8] Lymph node enlargement frequently (80%) occurs around the area of infection,[4] occurring seven to 10 days after chancre formation.[8] The lesion may persist for three to six weeks without treatment.[4]
Secondary[edit]


Secondary syphilis occurs approximately four to ten weeks after the primary infection.[4] While secondary disease is known for the many different ways it can manifest, symptoms most commonly involve the skin, mucous membranes, and lymph nodes.[9] There may be a symmetrical, reddish-pink, non-itchy rash on the trunk and extremities, including the palms and soles.[4][10] The rash may become maculopapular or pustular. It may form flat, broad, whitish, wart-like lesions known as condyloma latum on mucous membranes. All of these lesions harbor bacteria and are infectious. Other symptoms may include fever, sore throat, malaise, weight loss, hair loss, and headache.[4] Rare manifestations include hepatitis, kidney disease, arthritis, periostitis, optic neuritis, uveitis, and interstitial keratitis.[4][11] The acute symptoms usually resolve after three to six weeks;[11] however, about 25% of people may present with a recurrence of secondary symptoms. Many people who present with secondary syphilis (40–85% of women, 20–65% of men) do not report previously having had the classic chancre of primary syphilis.[9]
Latent[edit]
Latent syphilis is defined as having serologic proof of infection without symptoms of disease.[7] It is further described as either early (less than 1 year after secondary syphilis) or late (more than 1 year after secondary syphilis) in the United States.[11] The United Kingdom uses a cut-off of two years for early and late latent syphilis.[8] Early latent syphilis may have a relapse of symptoms. Late latent syphilis is asymptomatic, and not as contagious as early latent syphilis.[11]
Tertiary[edit]
Tertiary syphilis may occur approximately 3 to 15 years after the initial infection, and may be divided into three different forms: gummatous syphilis (15%), late neurosyphilis (6.5%), and cardiovascular syphilis (10%).[4][11] Without treatment, a third of infected people develop tertiary disease.[11] People with tertiary syphilis are not infectious.[4]

Gummatous syphilis or late benign syphilis usually occurs 1 to 46 years after the initial infection, with an average of 15 years. This stage is characterized by the formation of chronic gummas, which are soft, tumor-like balls of inflammation which may vary considerably in size. They typically affect the skin, bone, and liver, but can occur anywhere.[4]
Neurosyphilis refers to an infection involving the central nervous system. It may occur early, being either asymptomatic or in the form of syphilitic meningitis, or late as meningovascular syphilis, general paresis, or tabes dorsalis, which is associated with poor balance and lightning pains in the lower extremities. Late neurosyphilis typically occurs 4 to 25 years after the initial infection. Meningovascular syphilis typically presents with apathy and seizure, and general paresis with dementia and tabes dorsalis.[4] Also, there may be Argyll Robertson pupils, which are bilateral small pupils that constrict when the person focuses on near objects, but do not constrict when exposed to bright light.
Cardiovascular syphilis usually occurs 10–30 years after the initial infection. The most common complication is syphilitic aortitis, which may result in aneurysm formation.[4]
Congenital[edit]
Congenital syphilis may occur during pregnancy or during birth. Two-thirds of syphilitic infants are born without symptoms. Common symptoms that then develop over the first couple years of life include: hepatosplenomegaly (70%), rash (70%), fever (40%), neurosyphilis (20%), and pneumonitis (20%). If untreated, late congenital syphilis may occur in 40%, including: saddle nose deformation, Higoumenakis sign, saber shin, or Clutton's joints among others.[12]
Cause[edit]
Bacteriology[edit]

Treponema pallidum subspecies pallidum is a spiral-shaped, Gram-negative, highly mobile bacterium.[8][13] Three other human diseases are caused by related Treponema pallidum, including yaws (subspecies pertenue), pinta (subspecies carateum) and bejel (subspecies endemicum).[4] Unlike subtype pallidum, they do not cause neurological disease.[12] Humans are the only known natural reservoir for subspecies pallidum.[5] It is unable to survive without a host for more than a few days. This is due to its small genome (1.14 MDa) failing to encode the metabolic pathways necessary to make most of its macronutrients. It has a slow doubling time of greater than 30 hours.[8]
Transmission[edit]
Syphilis is transmitted primarily by sexual contact or during pregnancy from a mother to her fetus; the spirochaete is able to pass through intact mucous membranes or compromised skin.[4][5] It is thus transmissible by kissing near a lesion, as well as oral, vaginal, and anal sex.[4] Approximately 30 to 60% of those exposed to primary or secondary syphilis will get the disease.[11] Its infectivity is exemplified by the fact that an individual inoculated with only 57 organisms has a 50% chance of being infected.[8] Most (60%) of new cases in the United States occur in men who have sex with men. It can be transmitted via blood products. However, it is tested for in many countries and thus the risk is low. The risk of transmission from sharing needles appears limited.[4] Syphilis cannot be contracted through toilet seats, daily activities, hot tubs, or sharing eating utensils or clothing.[14]
Diagnosis[edit]

Syphilis is difficult to diagnose clinically early in its presentation.[8] Confirmation is either via blood tests or direct visual inspection using microscopy. Blood tests are more commonly used, as they are easier to perform.[4] Diagnostic tests are, however, unable to distinguish between the stages of the disease.[15]
Blood tests[edit]
Blood tests are divided into nontreponemal and treponemal tests.[8] Nontreponemal tests are used initially, and include venereal disease research laboratory (VDRL) and rapid plasma reagin tests. However, as these tests are occasionally false positives, confirmation is required with a treponemal test, such as treponemal pallidum particle agglutination (TPHA) or fluorescent treponemal antibody absorption test (FTA-Abs).[4] False positives on the nontreponemal tests can occur with some viral infections such as varicella and measles, as well as with lymphoma, tuberculosis, malaria, endocarditis, connective tissue disease, and pregnancy.[7] Treponemal antibody tests usually become positive two to five weeks after the initial infection.[8] Neurosyphilis is diagnosed by finding high numbers of leukocytes (predominately lymphocytes) and high protein levels in the cerebrospinal fluid in the setting of a known syphilis infection.[4][7]
Direct testing[edit]
Dark ground microscopy of serous fluid from a chancre may be used to make an immediate diagnosis. However, hospitals do not always have equipment or experienced staff members, whereas testing must be done within 10 minutes of acquiring the sample. Sensitivity has been reported to be nearly 80%, thus can only be used to confirm a diagnosis but not rule one out. Two other tests can be carried out on a sample from the chancre: direct fluorescent antibody testing and nucleic acid amplification tests. Direct fluorescent testing uses antibodies tagged with fluorescein, which attach to specific syphilis proteins, while nucleic acid amplification uses techniques, such as the polymerase chain reaction, to detect the presence of specific syphilis genes. These tests are not as time-sensitive, as they do not require living bacteria to make the diagnosis.[8]
Prevention[edit]
As of 2010[update], there is no vaccine effective for prevention.[5] Abstinence from intimate physical contact with an infected person is effective at reducing the transmission of syphilis, as is the proper use of a latex condom. Condom use, however, does not completely eliminate the risk.[14][16] Thus, the Centers for Disease Control and Prevention recommends a long-term, mutually monogamous relationship with an uninfected partner and the avoidance of substances such as alcohol and other drugs that increase risky sexual behavior.[14]
Congenital syphilis in the newborn can be prevented by screening mothers during early pregnancy and treating those who are infected.[17] The United States Preventive Services Task Force (USPSTF) strongly recommends universal screening of all pregnant women,[18] while the World Health Organization recommends all women be tested at their first antenatal visit and again in the third trimester.[19] If they are positive, they recommend their partners also be treated.[19] Congenital syphilis is, however, still common in the developing world, as many women do not receive antenatal care at all, and the antenatal care others do receive does not include screening,[17] and it still occasionally occurs in the developed world, as those most likely to acquire syphilis (through drug use, etc.) are least likely to receive care during pregnancy.[17] A number of measures to increase access to testing appear effective at reducing rates of congenital syphilis in low- to middle-income countries.[19]
Syphilis is a notifiable disease in many countries, including Canada[20] the European Union,[21] and the United States.[22] This means health care providers are required to notify public health authorities, which will then ideally provide partner notification to the person's partners. [23] Physicians may also encourage patients to send their partners to seek care.[24] The CDC recommends sexually active men who have sex with men are tested at least yearly.[25]
Treatment[edit]
Early infections[edit]
The first-choice treatment for uncomplicated syphilis remains a single dose of intramuscular penicillin G or a single dose of oral azithromycin.[26] Doxycycline and tetracycline are alternative choices; however, due to the risk of birth defects these are not recommended for pregnant women. Antibiotic resistance has developed to a number of agents, including macrolides, clindamycin, and rifampin.[5] Ceftriaxone, a third-generation cephalosporin antibiotic, may be as effective as penicillin-based treatment.[4]
Late infections[edit]
For neurosyphilis, due to the poor penetration of penicillin G into the central nervous system, those affected are recommended to be given large doses of intravenous penicillin for a minimum of 10 days.[4][5] If a person is allergic, ceftriaxone may be used or penicillin desensitization attempted. Other late presentations may be treated with once-weekly intramuscular penicillin G for three weeks. If allergic, as in the case of early disease, doxycycline or tetracycline may be used, albeit for a longer duration. Treatment at this stage limits further progression, but has only slight effect on damage which has already occurred.[4]
Jarisch-Herxheimer reaction[edit]
One of the potential side effects of treatment is the Jarisch-Herxheimer reaction. It frequently starts within one hour and lasts for 24 hours, with symptoms of fever, muscles pains, headache, and tachycardia.[4] It is caused by cytokines released by the immune system in response to lipoproteins released from rupturing syphilis bacteria.[27]
Epidemiology[edit]

| no data <35 35-70 70-105 105-140 140-175 175-210 | 210-245 245-280 280-315 315-350 350-500 >500 |
Syphilis is believed to have infected 12 million people in 1999, with greater than 90% of cases in the developing world.[5] It affects between 700,000 and 1.6 million pregnancies a year, resulting in spontaneous abortions, stillbirths, and congenital syphilis.[12] During 2010 it caused about 113,000 deaths down from 202,000 in 1990.[29] In sub-Saharan Africa, syphilis contributes to approximately 20% of perinatal deaths.[12] Rates are proportionally higher among intravenous drug users, those who are infected with HIV, and men who have sex with men.[1][2][3] In the United States, rates of syphilis as of 2007 were six times greater in men than women, while they were nearly equal in 1997.[30] African Americans accounted for almost half of all cases in 2010.[31]
Syphilis was very common in Europe during the 18th and 19th centuries. In the developed world during the early 20th century, infections declined rapidly with the widespread use of antibiotics, until the 1980s and 1990s.[13] Since the year 2000, rates of syphilis have been increasing in the USA, Canada, the UK, Australia and Europe, primarily among men who have sex with men.[5] Rates of syphilis among American women have, however, remained stable during this time, and rates among UK women have increased, but at a rate less than that of men.[32] Increased rates among heterosexuals have occurred in China and Russia since the 1990s.[5] This has been attributed to unsafe sexual practices, such as sexual promiscuity, prostitution, and decreasing use of barrier protection.[5][33][32]
Untreated, it has a mortality of 8% to 58%, with a greater death rate in males.[4] The symptoms of syphilis have become less severe over the 19th and 20th centuries, in part due to widespread availability of effective treatment and partly due to decreasing virulence of the spirochaete.[9] With early treatment, few complications result.[8] Syphilis increases the risk of HIV transmission by two to five times, and coinfection is common (30–60% in a number of urban centers).[4][5]
History[edit]

The exact origin of syphilis is disputed.[4] Syphilis was indisputably present in the Americas before European contact. The dispute is over whether or not syphilis was also present elsewhere in the world at that time. One of the two primary hypotheses proposes that syphilis was carried from the Americas to Europe by the returning crewmen from Christopher Columbus's voyage to the Americas. The other hypothesis says that syphilis existed in Europe previously, but went unrecognized until shortly after Columbus' return. These are referred to as the Columbian and pre-Columbian hypotheses, respectively.[15] The Columbian hypothesis is best supported by the available evidence.[35][36] The first written records of an outbreak of syphilis in Europe occurred in 1494 or 1495 in Naples, Italy, during a French invasion.[13][15] Due to its being spread by returning French troops, it was initially known as the "French disease." In 1530, the name "syphilis" was first used by the Italian physician and poet Girolamo Fracastoro as the title of his Latin poem in dactylic hexameter describing the ravages of the disease in Italy.[37] It was also known historically as the "Great Pox".[38][39]
The causative organism, Treponema pallidum, was first identified by Fritz Schaudinn and Erich Hoffmann in 1905.[13] The first effective treatment (Salvarsan) was developed in 1910 by Paul Ehrlich, which was followed by trials of penicillin and confirmation of its effectiveness in 1943.[13][38] Before the advent of effective treatment, mercury and isolation were commonly used, with treatments often worse than the disease.[38]
Many famous historical figures, including Franz Schubert, Arthur Schopenhauer, and Édouard Manet,[13] are believed to have had the disease.
Society and culture[edit]
Arts and literature[edit]
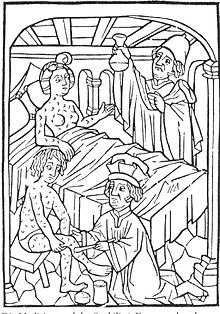
The earliest known depiction of an individual with syphilis is Albrecht Dürer's Syphilitic Man, a woodcut believed to represent a Landsknecht, a Northern European mercenary.[40] The myth of the femme fatale or "poison women" of the 19th century is believed to be partly derived from the devastation of syphilis, with classic examples in literature including John Keats' La Belle Dame sans Merci.[41][42]
The artist Jan van der Straet painted a scene of a wealthy man receiving treatment for syphilis with the tropical wood guaiacum sometime around 1580.[43] The title of the work is "Preparation and Use of Guayaco for Treating Syphilis". That the artist chose to include this image in a series of works celebrating the New World indicates how important a treatment, however ineffective, for syphilis was to the European elite at that time. The richly colored and detailed work depicts four servants preparing the concoction while a physician looks on, hiding something behind his back while the hapless patient drinks.[44]
Tuskegee and Guatemala studies[edit]
One of the most infamous United States cases of questionable medical ethics in the 20th century was the Tuskegee syphilis study.[45] The study took place in Tuskegee, Alabama, and was supported by the U.S. Public Health Service (PHS) in partnership with the Tuskegee Institute.[46] The study began in 1932, when syphilis was a widespread problem and there was no safe and effective treatment.[6] The study was designed to measure the progression of untreated syphilis. By 1947, penicillin had been validated as an effective cure for syphilis and was becoming widely used to treat the disease. Study directors, however, continued the study and did not offer the participants treatment with penicillin.[46] This is debated, and some have found that penicillin was given to many of the subjects.[6] The study did not end until 1972.[46]
Syphilis experiments were also carried out in Guatemala from 1946 to 1948. They were United States-sponsored human experiments, conducted during the government of Juan José Arévalo with the cooperation of some Guatemalan health ministries and officials. Doctors infected soldiers, prisoners, and mental patients with syphilis and other sexually transmitted diseases, without the informed consent of the subjects, and then treated them with antibiotics. In October 2010, the U.S. formally apologized to Guatemala for conducting these experiments.[47]
Syphilis Globally[edit]
The Reemergence of Syphilis around the World[edit]
China is a country that has suffered greatly from syphilis during the first part of the 20th century and basically eliminated the virus from 1960-1980. [48] During the 1950’s China was believed to have one of the worst cases of syphilis in human history. Different surveillance programs determined that 84% of Chinese prostitutes had the infection and as many as 5% of citizens had the disease in large cities. [49] The communist government under Mao Zedong, in response to the syphilis epidemic, issued free treatment for all those infected and increased screening for the disease. [50] In the 1960’s it was found that syphilis was almost completely eradicated in China. In recent studies there shows evidence that the disease has seen a resurgence. In a study titled Syphilis in China: Results of a National Surveillance Program researchers found that during 1993 the amount of cases of reported syphilis was 0-2 per 100,000. During a national surveillance program in 2005 there were found to be 5-7 cases per 100,000 throughout the country. [51] In that same study it showed that the city with the most prevalence of syphilis was in Shanghai with an estimated 55 patients with syphilis per 100,000 citizens. The second highest was Zhejiang which had approximately 35 people with syphilis per 100,000; the third was Fujian which had 28 patients per 100,000. [52] All of these cities are on the south-eastern edge of the country facing the ocean. The greatest increase in syphilis is in female sex workers, drug users, and gay men. [53] According to an article written in The Lancet titled “Syphilis Resurgent in China” the main cause of syphilis being more prevalent in China is due to the economic growth of China recently and increased globalization which has caused an increase of the sex trade, internal and external migration and a bigger economic inequality among its citizens. [54] Something else that is credited is that Chinas earlier efforts to control the disease helped increase the susceptibility of citizens to the disease. China’s increase in syphilis is not self-contained; Russia, the United Kingdom, Ireland the United States have all seen a great increase in patients with syphilis recently. Russia is one of the main areas around the world that has been affected by the syphilis epidemic. An article titled Epidemics of syphilis in the Russian Federation: trends, origins, and priorities for control written in The Lancet discussed trends of syphilis in Russia. Just like China, Russia basically eliminated the disease during the 1960’s; though there was a slight increase during 1978 and 1979 with an estimated 28 per 100,000 cases. The rate dropped slightly only to rise between 1988, where there were 4 patients per 100,000 citizens to 263 patients per 100,000 in 1996 which is 62 times more the amount then it previously was. [55] The most commonly effected individuals are found to be in young men and women. It is also reported that the estimated number of patients in Russia with syphilis who do not report their disease rose from around 0% in 1989 to 30% in 1993. [56] Many of the reasons for this increase in syphilis within Russia stem from political restructuring and a declining economy causing many people’s standard of living to go down. The gross national income of the country dropped roughly around 12% between 1990 and 1994. [57] The government funding of health services and social institutions went down and in turn caused less people to receive treatment for syphilis. This entire decline in the economy within Russia also led to an increase in the crossing of the country’s borders causing a mixing of surrounding area and more migration within and outside of Russia. [58] In Moscow especially a lot of travel has been done between other large cities. This increase in travel is in common with China’s increase in travel in recent years. Both have increased the number of sexual encounters with prostitutes and varied ideas of sexual ideology. Russia’s increased contact with the western world has brought more ideas on sexual orientation and an increase in pornography. [59] Russia right now is focused on making an increase in prevention and treatment programs throughout the country, making sure that the lower class of people have access to medical services and many health promotions are being made. [60] The United Kingdom and other parts of Western Europe have also seen a major increase in syphilis in recent times. A study called “Are trends in HIV, gonorrhea, and syphilis worsening in western Europe?” in a journal of medicine called BMJ outlines the data collected from 1995 to 2000 on sexually transmitted diseases throughout western Europe. As with Russia and China there was a big decline in syphilis before 1980 but a big resurgence during the 1990’s. [61] The most common form of how the disease was spread was from sex between two men, 37%, and the second highest was from sex between a man and a woman, 35%. Another major way of spreading the disease is the sharing of needles between drug users. [62] The Netherlands, Norway Ireland and France reported that most transmissions of syphilis were local and mainly between two men having sex. England and Wales saw a slight drop and then increase of syphilis cases between 1995 and 2000 and a drastic increase in syphilis contraction through homosexual men in 2000. [63] The increase in Western Europe can be attributed to the declining sexual morals of Western Europe with less safe sex practicing and young people are having more sex than they have had in the past. Due to a lack of modern surveillance programs and various governments in Europe there is not definitive data to show how prevalent the spread of syphilis is throughout every country in Western Europe. [64] The United States continued the trend seen throughout the globe with a sharp increase in syphilis during the 1990’s up till the present. The United States saw a big decrease in the number of cases in the 1950’s, with only around 6500 cases were reported per year, which was statistically about what other countries were seeing at the time. This continued with a varying increase around the 1960’s and 1970’s with around 19,000 and 26,000 cases per year up until the beginning of the 1990’s. [65] The center for disease control published their findings in 2013 with 19,738,800 almost 15% of those were from syphilis. It has been found that men and women are equally as likely to have syphilis in the United States. It is thought that the number of new cases of syphilis along with the current amount is around 117,000 people have syphilis in the United States. [66] To combat the increase in syphilis and other various sexually transmitted diseases the United States currently is focused on prevention programs where the focus is on practicing safe sex and being aware of whether ones partner has syphilis. Pregnant women, which are a high risk for spreading of the disease through their children, are required to take syphilis screening and given treatment if they are found to be carrying the disease. [67] All of these countries have in common a theme of travel in between countries which increases how prevalent and far reaching the disease can reach. Not only is travel linked to the reemergence of syphilis but also the Internet has been a major factor in syphilis being transferred from person to person. A study done in 2000 titled “Tracing a Syphilis Outbreak Through Cyberspace” published in The Journal of American Medical Association shows that Internet chat rooms increase the frequency of sexual contact between people, especially those of gay men. [68] In a specific outbreak in San Francisco gay men with syphilis were found to be a lot more probable to have met their significant other through the Internet. The ratio was found to be that 67% of the men met their partner through an Internet chat room and only 19% of those with reported syphilis were not linked to the Internet. [69] The Internet is a global force that facilitates sexual encounters among people which spreads the disease to many people who otherwise would not be in contact with syphilis. This global re-emergence of syphilis is a major problem for every country affected. According to a study titled “Global Prevalence and Incidence Estimates of Selectable Curable STD’s” in a journal named Sex Transm Inf the amount of syphilis cases reported within the 9 main UN territories in 1995 was roughly around 12 million cases. [70] The main population that was reported to have the disease was the people who were lower in the economy and younger people are reported to have more of the disease than older people. 1. I think that the Gettysburg Address has contemporary relavence for a couple reasons. The first is that it teaches us about how a true American really should reflect on what was said during the speech. Another reason that it is relavent in modern times is because this was a major part of our history and forgetting it would be a disservice for all that it represented. Out of the nine UN regions that were surveyed the region that syphilis was the most prevalent was south and south eastern Asia. The second highest was found to be in the sub Saharan parts of Africa and the third highest was Latin America and the Caribbean areas. [71] This study in 1995 was one of the first big attempts by the World Health Organization to find a good estimate of the total population of people with syphilis and other STD’s. More recently in studies done by the World Health Organization pinpoint how prevalent syphilis is globally. An article called “Congenital syphilis re-emerging” in a medical journal titled JDDG outlines the World Health Organizations findings as recently as 2008. It is estimated that globally 12 million people acquire the disease every year and of these 12 million patients 2 million are pregnant women. [72] This high amount of pregnant women with the disease estimates that it will cause about 50% of the pregnancies to result in stillbirths or prenatal deaths. The World Health Organization estimates that syphilis in within the mother can cause syphilis in the baby between 713,600 cases and 1,575,000 cases. [73] Because of the increased numbers of patients globally there have been many initiatives to prevent the spread of the disease and there has been a global effort to eradicate the disease. An article titled “A Road Map for the Global Elimination of Congenital Syphilis” within a medical journal called Obstetrics and Gynecology International outlines the global efforts to combat congenital syphilis mostly dealing with the World Health Organization. Many of the efforts are focused on screening women who are pregnant for the disease and treating them. [74] Of the two million pregnancies each year that test positive for syphilis they make up 1.5% of every pregnancy throughout the world. [75] During 2007 the World Health Organization estimated in 2007 that in the countries that are affected most by congenital syphilis it would cost roughly 3 to 4 million dollars to start a program that could potentially eliminate most of the threat of congenital syphilis by focusing a lot more on screening and treatment. [76] Sub Saharan countries in Africa find it difficult to implement these kinds of treatment due to a lack of health services for its citizens which in turn makes this area a big breeding ground for congenital syphilis and the spread of syphilis through sexual contact. The World Health Organization outlines a four pillared plan that if stuck to can help countries eliminate or at least decrease the numbers of cases of congenital syphilis. The four pillars are “ensure advocacy and sustained political commitment for a successful health initiative, increase access to, and quality of, maternal and newborn health services, screen and treat pregnant women and partners, and establish surveillance, monitoring, and evaluation systems.” [77] . The United Nations has also added goals related to the lowering of syphilis which they call the Millennium Development Goals. These goals include reducing infant death from syphilis and increasing the health of mothers with syphilis. [78] The United Nations have taken steps to include on site screening and testing for syphilis among other sexually transmitted diseases along with an increase in partner notification. The global effort to stop the reemergence of syphilis is seen throughout every country and syphilis is becoming a more stable virus than what was seen in the very recent past.
References[edit]
- ^ a b Coffin, Lara S.; Newberry, Ashley; Hagan, Holly; Cleland, Charles M.; Des Jarlais, Don C.; Perlman, David C. (January 2010). "Syphilis in Drug Users in Low and Middle Income Countries". The International Journal on Drug Policy. 21 (1): 20–7. doi:10.1016/j.drugpo.2009.02.008. PMC 2790553. PMID 19361976.
- ^ a b Gao, L.; Zhang, L.; Jin, Q. (September 2009). "Meta-analysis: prevalence of HIV infection and syphilis among MSM in China". Sexually Transmitted Infections. 85 (5): 354–8. doi:10.1136/sti.2008.034702. PMID 19351623.
- ^ a b Karp, Galia; Schlaeffer, Francisc; Jotkowitz, Alan; Riesenberg, Klaris (January 2009). "Syphilis and HIV co-infection". European Journal of Internal Medicine. 20 (1): 9–13. doi:10.1016/j.ejim.2008.04.002. PMID 19237085.
- ^ a b c d e f g h i j k l m n o p q r s t u v w x y z aa ab ac ad Kent ME, Romanelli F (February 2008). "Reexamining syphilis: an update on epidemiology, clinical manifestations, and management". Annals of Pharmacotherapy. 42 (2): 226–36. doi:10.1345/aph.1K086. PMID 18212261.
{{cite journal}}: CS1 maint: date and year (link) - ^ a b c d e f g h i j k Stamm LV (February 2010). "Global Challenge of Antibiotic-Resistant Treponema pallidum" (PDF). Antimicrob. Agents Chemother. 54 (2): 583–9. doi:10.1128/AAC.01095-09. PMC 2812177. PMID 19805553.
{{cite journal}}: CS1 maint: date and year (link) - ^ a b c White, RM (13 March 2000). "Unraveling the Tuskegee Study of Untreated Syphilis". Archives of Internal Medicine. 160 (5): 585–98. doi:10.1001/archinte.160.5.585. PMID 10724044.
- ^ a b c d Committee on Infectious Diseases (2006). Larry K. Pickering (ed.). Red book 2006 Report of the Committee on Infectious Diseases (27th ed.). Elk Grove Village, IL: American Academy of Pediatrics. pp. 631–44. ISBN 978-1-58110-207-9.
- ^ a b c d e f g h i j k l m Eccleston, Kathryn; Collins, Lisa; Higgins, Stephen P. (March 2008). "Primary syphilis". International Journal of STD & AIDS. 19 (3): 145–51. doi:10.1258/ijsa.2007.007258. PMID 18397550.
- ^ a b c Mullooly, C.; Higgins, S. P. (August 2010). "Secondary syphilis: the classical triad of skin rash, mucosal ulceration and lymphadenopathy". International Journal of STD & AIDS. 21 (8): 537–45. doi:10.1258/ijsa.2010.010243. PMID 20975084.
- ^ Dylewski J, Duong M (2 January 2007). "The rash of secondary syphilis". Canadian Medical Association Journal. 176 (1): 33–5. doi:10.1503/cmaj.060665. PMC 1764588. PMID 17200385.
- ^ a b c d e f g Bhatti MT (2007). "Optic neuropathy from viruses and spirochetes". Int Ophthalmol Clin. 47 (4): 37–66, ix. doi:10.1097/IIO.0b013e318157202d. PMID 18049280.
- ^ a b c d Woods CR (June 2009). "Congenital syphilis-persisting pestilence". Pediatr. Infect. Dis. J. 28 (6): 536–7. doi:10.1097/INF.0b013e3181ac8a69. PMID 19483520.
{{cite journal}}: CS1 maint: date and year (link) - ^ a b c d e f Franzen, C (December 2008). "Syphilis in composers and musicians--Mozart, Beethoven, Paganini, Schubert, Schumann, Smetana". European Journal of Clinical Microbiology and Infectious Diseases. 27 (12): 1151–7. doi:10.1007/s10096-008-0571-x. PMID 18592279.
- ^ a b c "Syphilis - CDC Fact Sheet". Centers for Disease Control and Prevention (CDC). 16 September 2010. Retrieved 30 May 2007.
- ^ a b c Farhi, David; Dupin, Nicolas (September 2010-Oct). "Origins of syphilis and management in the immunocompetent patient: facts and controversies". Clinics in Dermatology. 28 (5): 533–8. doi:10.1016/j.clindermatol.2010.03.011. PMID 20797514.
{{cite journal}}: Check date values in:|date=(help) - ^ Koss CA, Dunne EF, Warner L (July 2009). "A systematic review of epidemiologic studies assessing condom use and risk of syphilis". Sex Transm Dis. 36 (7): 401–5. doi:10.1097/OLQ.0b013e3181a396eb. PMID 19455075.
{{cite journal}}: CS1 maint: date and year (link) CS1 maint: multiple names: authors list (link) - ^ a b c Schmid, G (June 2004). "Economic and programmatic aspects of congenital syphilis prevention". Bulletin of the World Health Organization. 82 (6): 402–9. PMC 2622861. PMID 15356931.
- ^ U.S. Preventive Services Task, Force (May 2009 19). "Screening for syphilis infection in pregnancy: U.S. Preventive Services Task Force reaffirmation recommendation statement". Annals of Internal Medicine. 150 (10): 705–9. doi:10.7326/0003-4819-150-10-200905190-00008. PMID 19451577.
{{cite journal}}: Check date values in:|date=(help) - ^ a b c Hawkes, Sarah; Matin, Nashaba; Broutet, Nathalie; Low, Nicola (June 2011 15). "Effectiveness of interventions to improve screening for syphilis in pregnancy: a systematic review and meta-analysis". The Lancet Infectious Diseases. 11 (9): 684–91. doi:10.1016/S1473-3099(11)70104-9. PMID 21683653.
{{cite journal}}: Check date values in:|date=(help) - ^ "National Notifiable Diseases". Public Health Agency of Canada. 5 April 2005. Retrieved 2 August 2011.
- ^ Viñals-Iglesias, H.; Chimenos-Küstner, E. (September 2009 1). "The reappearance of a forgotten disease in the oral cavity: syphilis". Medicina Oral, Patologia Oral y Cirugia Bucal. 14 (9): e416–20. PMID 19415060.
{{cite journal}}: Check date values in:|date=(help) - ^ "Table 6.5. Infectious Diseases Designated as Notifiable at the National Level-United States, 2009 [a]". Red Book. Retrieved 2 August 2011.
- ^ Brunner & Suddarth's textbook of medical-surgical nursing (12th ed.). Philadelphia: Wolters Kluwer Health/Lippincott Williams & Wilkins. 2010. p. 2144. ISBN 978-0-7817-8589-1.
- ^ Hogben, M (April 2007 1). "Partner notification for sexually transmitted diseases". Clinical Infectious Diseases: An Official Publication of the Infectious Diseases Society of America. 44 (Suppl 3): S160–74. doi:10.1086/511429. PMID 17342669.
{{cite journal}}: Check date values in:|date=(help) - ^ "Trends in Sexually Transmitted Diseases in the United States: 2009 National Data for Gonorrhea, Chlamydia and Syphilis". Centers for Disease Control and Prevention. 22 November 2010. Retrieved 3 August 2011.
- ^ David N. Gilbert; Robert C. Moellering; George M. Eliopoulos (2 August 2023). The Sanford guide to antimicrobial therapy 2011 (41st ed.). Sperryville, VA: Antimicrobial Therapy. p. 22. ISBN 978-1-930808-65-2.
{{cite book}}: Invalid|display-authors=3(help); Unknown parameter|author-separator=ignored (help) - ^ Radolf, JD; Lukehart SA (editors) (2006). Pathogenic Treponema: Molecular and Cellular Biology. Caister Academic Press. ISBN 1-904455-10-7.
{{cite book}}:|author=has generic name (help)CS1 maint: multiple names: authors list (link) - ^ "Disease and injury country estimates". World Health Organization (WHO). 2004. Retrieved 11 November 2009.
- ^ Lozano, R (2012 Dec 15). "Global and regional mortality from 235 causes of death for 20 age groups in 1990 and 2010: a systematic analysis for the Global Burden of Disease Study 2010". Lancet. 380 (9859): 2095–128. doi:10.1016/S0140-6736(12)61728-0. PMID 23245604.
{{cite journal}}: Check date values in:|date=(help) - ^ "Trends in Reportable Sexually Transmitted Diseases in the United States, 2007". Centers for Disease Control and Prevention (CDC). 13 January 2009. Retrieved 2 August 2011.
- ^ "STD Trends in the United States: 2010 National Data for Gonorrhea, Chlamydia, and Syphilis". Centers for Disease Control and Prevention (CDC). 22 November 2010. Retrieved 20 November 2011.
- ^ a b Kent, Molly E.; Romanelli, Frank (February 2008). "Reexamining syphilis: an update on epidemiology, clinical manifestations, and management". Annals of Pharmacotherapy. 42 (2): 226–36. doi:10.1345/aph.1K086. PMID 18212261.
- ^ Ficarra, Giuseppe; Carlos, Roman (September 2009). "Syphilis: The Renaissance of an Old Disease with Oral Implications". Head and Neck Pathology. 3 (3): 195–206. doi:10.1007/s12105-009-0127-0. PMC 2811633. PMID 20596972.
- ^ The Metropolitan Museum of Art Bulletin, Summer 2007, pp. 55–56.
- ^ Rothschild, BM (15 May 2005). "History of syphilis". Clinical Infectious Diseases: An Official Publication of the Infectious Diseases Society of America. 40 (10): 1454–63. doi:10.1086/429626. PMID 15844068.
- ^ Harper, Kristin N.; Zuckerman, Molly K.; Harper, Megan L.; Kingston, John D.; Armelagos, George J. (2011). "The origin and antiquity of syphilis revisited: an appraisal of Old World pre-Columbian evidence for treponemal infection". American Journal of Physical Anthropology. 146 (Suppl 53): 99–133. doi:10.1002/ajpa.21613. PMID 22101689.
{{cite journal}}: CS1 maint: date and year (link) - ^ Nancy G. "Siraisi, Drugs and Diseases: New World Biology and Old World Learning," in Anthony Grafton, Nancy G. Siraisi, with April Shelton, eds. (1992). New World, Ancient Texts (Cambridge MA: Belknap Press/Harvard University Press), pages 159-194
- ^ a b c Dayan, Linda; Ooi, Catriona (October 2005). "Syphilis treatment: old and new". Expert Opinion on Pharmacotherapy. 6 (13): 2271–80. doi:10.1517/14656566.6.13.2271. PMID 16218887.
- ^ Knell, RJ (7 May 2004). "Syphilis in renaissance Europe: rapid evolution of an introduced sexually transmitted disease?" (PDF). Proceedings. Biological Sciences / The Royal Society. 271 (Suppl 4): S174–6. doi:10.1098/rsbl.2003.0131. PMC 1810019. PMID 15252975.
- ^ Eisler, CT (2009 Winter). "Who is Dürer's "Syphilitic Man"?". Perspectives in Biology and Medicine. 52 (1): 48–60. doi:10.1353/pbm.0.0065. PMID 19168944.
{{cite journal}}: Check date values in:|date=(help) - ^ Hughes, Robert (2007). Things I didn't know : a memoir (1st Vintage Book ed.). New York: Vintage. p. 346. ISBN 978-0-307-38598-7.
- ^ Wilson, [ed]: Joanne Entwistle, Elizabeth (2005). Body dressing ([Online-Ausg.] ed.). Oxford: Berg Publishers. p. 205. ISBN 978-1-85973-444-5.
{{cite book}}:|first=has generic name (help)CS1 maint: multiple names: authors list (link) - ^ Reid, Basil A. (2009). Myths and realities of Caribbean history ([Online-Ausg.] ed.). Tuscaloosa: University of Alabama Press. p. 113. ISBN 978-0-8173-5534-0.
- ^ "Preparation and Use of Guayaco for Treating Syphilis". Jan van der Straet. Retrieved 6 August 2007.
- ^ Katz RV; Kegeles SS; Kressin NR; et al. (November 2006). "The Tuskegee Legacy Project: Willingness of Minorities to Participate in Biomedical Research". J Health Care Poor Underserved. 17 (4): 698–715. doi:10.1353/hpu.2006.0126. PMC 1780164. PMID 17242525.
{{cite journal}}: Unknown parameter|author-separator=ignored (help)CS1 maint: date and year (link) - ^ a b c "U.S. Public Health Service Syphilis Study at Tuskegee". Centers for Disease Control and Prevention. 15 June 2011. Retrieved 7 July 2010.
- ^ "U.S. apologizes for newly revealed syphilis experiments done in Guatemala". The Washington Post. 1 October 2010. Retrieved 1 October 2010.
The United States revealed on Friday that the government conducted medical experiments in the 1940s in which doctors infected soldiers, prisoners and mental patients in Guatemala with syphilis and other sexually transmitted diseases.
{{cite news}}: Cite has empty unknown parameter:|coauthors=(help) - ^ Chen, Zhang (2007). "Syphilis in China: Results of a national surveillance programme". The Lancet. 369 (9556): 132–138. doi:10.1016/S0140-6736(07)60074-9. PMC 7138057. PMID 17223476.
- ^ Chen, Zhang (2007). "Syphilis in China: Results of a national surveillance programme". The Lancet. 369 (9556): 132–138. doi:10.1016/S0140-6736(07)60074-9. PMC 7138057. PMID 17223476.
- ^ Chen, Zhang (2007). "Syphilis in China: Results of a national surveillance programme". The Lancet. 369 (9556): 132–138. doi:10.1016/S0140-6736(07)60074-9. PMC 7138057. PMID 17223476.
- ^ Chen, Zhang (2007). "Syphilis in China: Results of a national surveillance programme". The Lancet. 369 (9556): 132–138. doi:10.1016/S0140-6736(07)60074-9. PMC 7138057. PMID 17223476.
- ^ Chen, Zhang (2007). "Syphilis in China: Results of a national surveillance programme". The Lancet. 369 (9556): 132–138. doi:10.1016/S0140-6736(07)60074-9. PMC 7138057. PMID 17223476.
- ^ Chen, Zhang (2007). "Syphilis in China: Results of a national surveillance programme". The Lancet. 369 (9556): 132–138. doi:10.1016/S0140-6736(07)60074-9. PMC 7138057. PMID 17223476.
- ^ Fisman, D. (2007). "Syphilis Resurgent in China". The Lancet. 369 (9556): 84–85. doi:10.1016/S0140-6736(07)60044-0. PMID 17223453.
- ^ Tichonova, L (1997). "Epidemics of syphilis in the Russian Federation: Trends, origins, and priorities for control". The Lancet. 350 (9072): 210–213. doi:10.1016/S0140-6736(97)01382-2. PMID 9250199.
- ^ Tichonova, L (1997). "Epidemics of syphilis in the Russian Federation: Trends, origins, and priorities for control". The Lancet. 350 (9072): 210–213. doi:10.1016/S0140-6736(97)01382-2. PMID 9250199.
- ^ Tichonova, L (1997). "Epidemics of syphilis in the Russian Federation: Trends, origins, and priorities for control". The Lancet. 350 (9072): 210–213. doi:10.1016/S0140-6736(97)01382-2. PMID 9250199.
- ^ Tichonova, L (1997). "Epidemics of syphilis in the Russian Federation: Trends, origins, and priorities for control". The Lancet. 350 (9072): 210–213. doi:10.1016/S0140-6736(97)01382-2. PMID 9250199.
- ^ Tichonova, L (1997). "Epidemics of syphilis in the Russian Federation: Trends, origins, and priorities for control". The Lancet. 350 (9072): 210–213. doi:10.1016/S0140-6736(97)01382-2. PMID 9250199.
- ^ Tichonova, L (1997). "Epidemics of syphilis in the Russian Federation: Trends, origins, and priorities for control". The Lancet. 350 (9072): 210–213. doi:10.1016/S0140-6736(97)01382-2. PMID 9250199.
- ^ Nicoll, A (2002). "Are trends in HIV, gonorrhoea, and syphilis worsening in western Europe?". BMJ. 324 (7349): 1324–1327. doi:10.1136/bmj.324.7349.1324. PMC 1123279. PMID 12039830.
- ^ Nicoll, A (2002). "Are trends in HIV, gonorrhoea, and syphilis worsening in western Europe?". BMJ. 324 (7349): 1324–1327. doi:10.1136/bmj.324.7349.1324. PMC 1123279. PMID 12039830.
- ^ Nicoll, A (2002). "Are trends in HIV, gonorrhoea, and syphilis worsening in western Europe?". BMJ. 324 (7349): 1324–1327. doi:10.1136/bmj.324.7349.1324. PMC 1123279. PMID 12039830.
- ^ Nicoll, A (2002). "Are trends in HIV, gonorrhoea, and syphilis worsening in western Europe?". BMJ. 324 (7349): 1324–1327. doi:10.1136/bmj.324.7349.1324. PMC 1123279. PMID 12039830.
- ^ Hook, E (1992). "Acquired Syphilis in Adults". The New England Journal of Medicine. 326 (16): 1060–1070. doi:10.1056/NEJM199204163261606. PMID 1549153.
- ^ "Sexually Transmitted Diseases". Center for Disease Control.
- ^ "Sexually Transmitted Diseases". Center for Disease Control.
- ^ Klausner, J (2000). "Tracing a Syphilis Outbreak Through Cyberspace". The Journal of the American Medical Association. 284 (4): 447–449. doi:10.1001/jama.284.4.447. PMID 10904507.
- ^ Klausner, J (2000). "Tracing a Syphilis Outbreak Through Cyberspace". The Journal of the American Medical Association. 284 (4): 447–449. doi:10.1001/jama.284.4.447. PMID 10904507.
- ^ Gerbase, A (1998). "Global prevelance and incidence estimates of selected curable stds" (PDF). Sex Trasm Inf. 74: 12–16.
- ^ Gerbase, A (1998). "Global prevelance and incidence estimates of selected curable stds" (PDF). Sex Trasm Inf. 74: 12–16.
- ^ Simms, I (2008). "Congenital syphilis re-emerging". JDDG. 6 (4): 269–272. doi:10.1111/j.1610-0387.2008.06490.x. PMID 18266865.
- ^ Simms, I (2008). "Congenital syphilis re-emerging". JDDG. 6 (4): 269–272. doi:10.1111/j.1610-0387.2008.06490.x. PMID 18266865.
- ^ Kamb, M (2010). "A Road Map for the Global Elimination of Congenital Syphilis". Obstetrics and Gynecology International. 2010: 1–6. doi:10.1155/2010/312798. PMC 2913802. PMID 20706693.
- ^ Kamb, M (2010). "A Road Map for the Global Elimination of Congenital Syphilis". Obstetrics and Gynecology International. 2010: 1–6. doi:10.1155/2010/312798. PMC 2913802. PMID 20706693.
- ^ Kamb, M (2010). "A Road Map for the Global Elimination of Congenital Syphilis". Obstetrics and Gynecology International. 2010: 1–6. doi:10.1155/2010/312798. PMC 2913802. PMID 20706693.
- ^ Kamb, M (2010). "A Road Map for the Global Elimination of Congenital Syphilis". Obstetrics and Gynecology International. 2010: 1–6. doi:10.1155/2010/312798. PMC 2913802. PMID 20706693.
- ^ Simms, I (2008). "Congenital syphilis re-emerging". JDDG. 6 (4): 269–272. doi:10.1111/j.1610-0387.2008.06490.x. PMID 18266865.
Further reading[edit]
- Parascandola, John. Sex, Sin, and Science: A History of Syphilis in America (Praeger, 2008) 195 pp. ISBN 978-0-275-99430-3 excerpt and text search
- Shmaefsky, Brian, Hilary Babcock and David L. Heymann. Syphilis (Deadly Diseases & Epidemics) (2009)
- Stein, Claudia. Negotiating the French Pox in Early Modern Germany (2009)
External links[edit]
- "Syphilis - CDC Fact Sheet" Centers for Disease Control and Prevention (CDC)
- UCSF HIV InSite Knowledge Base Chapter: Syphilis and HIV
Category:Bacterial diseases Category:Bacterium-related cutaneous conditions Category:Infections with a predominantly sexual mode of transmission Category:Spirochaetes

