User:SewellBio/sandbox
 | This is a user sandbox of SewellBio. You can use it for testing or practicing edits. This is not the sandbox where you should draft your assigned article for a dashboard.wikiedu.org course. To find the right sandbox for your assignment, visit your Dashboard course page and follow the Sandbox Draft link for your assigned article in the My Articles section. |
History[edit]
Foix-Chavany-Marie (SFMC) syndrome was termed in a literature review proposed by Weller in 1993. This review allowed the etiological classification of SFMC into five clinical subtypes; Classical, Subacute, Developmental, Reversible, and Chronic.[1] Weller termed SFMC in recognition of Charles Foix, Jean Alfred Emile Chavany, and Julien Marie. French Physicians, Foix et al. introduced pseudobulbar palsy resulting from bilateral opecular lesions, a syndrome later termed SFMC, to Neurological literature in 1926. The published journal in Revenue Neurologique described the facio-labio-pharngo-maticatory paralysis and automatic- voluntary dissociation characteristic of SFMC.[2] Prior to this introduction, case reports on SFMC were confined to French literature. The development of computer tomography imaging techniques, such as CT and MRI, expanded publications on SFMC to Anglo-American literature.[3]
| Operculum (brain) | |
|---|---|
 Operculum | |
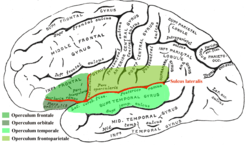
 Frontal (coronal) section of the human brain. Lesions occurring in the highlighted regions are characteristic of Foix-Chavany-Marie Syndrome. | |
| Anatomical terms of neuroanatomy |
The first case report of SFMC was documented in 1837 by Magnus, a German physician. Magnus documented his postmortem observations describing features characteristic of pseudobulbar palsy following multiple infarcts (necrosis of brain tissue following ischemic attacks).[4] The term pseudobulbar palsy was coined in 1877 by Lepine to describe lower cranial nerve palsy or paralysis induced by supranuclear lesions, which included corticobulbar and corticopontine lesions. This created a distinction from motor paralysis that may occur following damage to the brainstem nuclei. Additional clinical and anatomic studies during the onset the twentieth century led to the publication of Thurel’s thesis in 1929. Thurel subdivided pseudobulbar palsy into three subtypes; Cortical, Striatal, and Pontine. The pseudobulbar palsy described by Magnus and later investigated by Foix et al was classified as the cortical form characterized by faciopharyngoglossomasticatory deplegia with automatic voluntary dissociation.[5]
Treatment[edit]
Treatment of Foix-Chavany-Marie syndrome depends on the onset of symptoms and involves a multidisciplinary approach. Drugs are used in neurological recovery depending on the etiological classification of SFMC. Reversible SFMC, specifically resulting in the development of lesions in the bilateral and subcortical regions of the brain can be treated using antiepileptic drugs to reverse abnormal EEG changes and induce complete neurological recovery.[6] Physical Therapy is also used to manage symptoms and improve quality of life. For instance, in classical SFMC resulting in the decline of ones ability to speak and swallow treated with neuromuscular electrical stimulation and traditional dysphagia therapy improves oral feeding. Modified feeding techniques and postures also aid in recovery.[7]
References[edit]
- ^ Laurent-vannier A, Fadda G, Laigle P, Dusser A, Leroy-malherbe V. [Foix-Chavany-Marie syndrome in a child caused by a head trauma]. Rev Neurol (Paris). 1999;155(5):387-90.
- ^ Foix, Charles; Jean Alfred Émile Chavany; Julien Marie (1926). "Diplégie facio-linguo-masticatrice d'origine sous-corticale sans paralysie des membres (contribution à l'étude de la localisation des centres de la face du membre supérieur)". Revue neurologique. 33: 214–219.
- ^ Christen HJ, Hanefeld F, Kruse E, Imhäuser S, Ernst JP, Finkenstaedt M. Foix-Chavany-Marie (anterior operculum) syndrome in childhood: a reappraisal of Worster-Drought syndrome. Dev Med Child Neurol. 2000;42(2):122-32.
- ^ Hesser F, Longworthy. [SYNDROME OF PSEUDOBULBAR PALSY AN ATOMIC AND PHYSIOLOGICAL ANALYSIS. Arch Intern Med (Chic). 1940;65(1):106-121.
- ^ Besson G, Bogousslavsky J, Regli F, Maeder P. Acute pseudobulbar or suprabulbar palsy. Arch Neurol. 1991;48(5):501-7.
- ^ Lekhjung T, Raju Paudel, Rana PVS. [Opercular syndrome: Case reports and review of literature]. Neurology Asia. 2010; 15(2): 145-152.
- ^ Chernev I, Petrea R, Reynolds M, Wang F.[The Classical Type of Foix-Chavany-Marie Syndrome: Assessment and Treatment of Dysphagia]. The Internet Journal of Neurology. 2008 Volume 11 Number 1.
