User:Mr. Ibrahem/Toxic shock syndrome
| Toxic shock syndrome | |
|---|---|
| Other names | Staphylococcal scarlet fever;[1] bacterial toxic shock syndrome[2] |
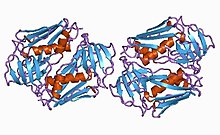 | |
| Toxic shock syndrome toxin-1 protein from staphylococcus | |
| Specialty | Infectious disease |
| Symptoms | Fever, rash, skin peeling, low blood pressure[3] |
| Usual onset | Rapid[3] |
| Types | Staphylococcal (menstrual and nonmenstrual), streptococcal[3] |
| Causes | Streptococcus pyogenes, Staphylococcus aureus, others[3][4] |
| Risk factors | Very absorbent tampons, skin lesions in young children[3] |
| Diagnostic method | Based on symptoms[3] |
| Differential diagnosis | Septic shock, Kawasaki's disease, Stevens–Johnson syndrome, scarlet fever[5] |
| Treatment | Antibiotics, incision and drainage of any abscesses, intravenous immunoglobulin[3] |
| Prognosis | Risk of death: ~50% (streptococcal), ~5% (staphylococcal)[3] |
| Frequency | 3 per 100,000 per year (developed world)[3] |
Toxic shock syndrome (TSS) is a condition caused by bacterial toxins.[3] Symptoms may include fever, rash, skin peeling, and low blood pressure.[3] There may also be symptoms related to the specific underlying infection such as mastitis, osteomyelitis, necrotising fasciitis, or pneumonia.[3]
TSS is typically caused by bacteria of the Streptococcus pyogenes or Staphylococcus aureus type, though others may also be involved.[3][4] Streptococcal toxic shock syndrome is sometimes referred to as toxic-shock-like syndrome (TSLS).[3] The underlying mechanism involves the production of superantigens during an invasive streptococcus infection or a localized staphylococcus infection.[3] Risk factors for the staphylococcal type include the use of very absorbent tampons, and skin lesions in young children.[3] Diagnosis is typically based on symptoms.[3]
Treatment includes intravenous fluids, antibiotics, incision and drainage of any abscesses, and possibly intravenous immunoglobulin.[3][6] The need for rapid removal of infected tissue via surgery in those with a streptococcal cause, while commonly recommended, is poorly supported by the evidence.[3] Some recommend delaying surgical debridement.[3] The overall risk of death is about 50% in streptococcal disease, and 5% in staphylococcal disease.[3] Death may occur within 2 days.[3]
In the United States streptococcal TSS occurs in about 3 per 100,000 per year, and staphylococcal TSS in about 0.5 per 100,000 per year.[3] The condition is more common in the developing world.[3] It was first described in 1927.[3] Due to the association with very absorbent tampons, these products were removed from sale.[3]
References[edit]
- ^ "Toxic shock syndrome | DermNet". dermnetnz.org. Archived from the original on 24 November 2022. Retrieved 21 December 2022.
- ^ RESERVED, INSERM US14-- ALL RIGHTS. "Orphanet: Bacterial toxic shock syndrome". www.orpha.net. Archived from the original on 29 November 2023. Retrieved 15 February 2024.
{{cite web}}: CS1 maint: numeric names: authors list (link) - ^ a b c d e f g h i j k l m n o p q r s t u v w x y z Low, DE (July 2013). "Toxic shock syndrome: major advances in pathogenesis, but not treatment". Critical Care Clinics. 29 (3): 651–75. doi:10.1016/j.ccc.2013.03.012. PMID 23830657.
- ^ a b Gottlieb, Michael; Long, Brit; Koyfman, Alex (June 2018). "The Evaluation and Management of Toxic Shock Syndrome in the Emergency Department: A Review of the Literature". The Journal of Emergency Medicine. 54 (6): 807–814. doi:10.1016/j.jemermed.2017.12.048. PMID 29366615.
- ^ Ferri, Fred F. (2010). Ferri's differential diagnosis : a practical guide to the differential diagnosis of symptoms, signs, and clinical disorders (2nd ed.). Philadelphia: Elsevier/Mosby. p. Chapter T. ISBN 978-0323076999.
- ^ Wilkins, Amanda L.; Steer, Andrew C.; Smeesters, Pierre R.; Curtis, Nigel (2017). "Toxic shock syndrome – the seven Rs of management and treatment". Journal of Infection. 74: S147–S152. doi:10.1016/S0163-4453(17)30206-2. PMID 28646955.
