User:Knotwhite/Drugs and Sexual Performance
Drugs and Sexual Performance refers to the influence of substances on sexual function and experience. Sexual performance is known as the execution of the act of sex and the quality of sexual activity. This includes elements such as libido (a person's sexual drive), sexual function (including erection in males and vaginal lubrication in females), sensation (the ability to achieve orgasm). Drugs are termed as any chemical substance that produces a physiological and or psychological change in an organism. Drugs categorized as psychoactive drugs, antihypertensive drugs, antihistamines, cancer treatment, and hormone medication have a significant impact on sexual performance. Various drugs result in different effects, both positive and negative. Negative effects may include low libido, erection issues (in males), vaginal dryness (in females) and anorgasmia. Positive effects usually address these issues, overall enhancing sexual performance and contributing to a more enjoyable sexual experience. It is crucial to know that the impact of drugs on sexual performance varies among individuals, especially among different genders.
Understanding sexual performance[edit]
Understanding sexual performance involves recognizing various factors that are responsible for a person’s combined sexual experience and function. This includes libido, a person’s overall sexual desire, and drive; sexual function, which encompasses the male’s erectile function and a female’s vaginal lubrication; and sensations, which in this context refers to a person’s ability to have orgasms and/or ejaculations.
Libido[edit]
Libido is primarily regulated by the hypothalamus, where sex hormones (testosterone and estrogen), and neurotransmitters (dopamine, oxytocin and serotonin), are the main components that influence sex drive[1][2]. A decreased libido is predominantly caused by low testosterone in males[2]. For females, serotonin acts as a inhibitor for sexual desire as it reduces the ability of stimulatory systems for sexual cues[3].
Sexual function[edit]

Penile erection for men is a vascular event caused by the innervation of both autonomic (sympathetic and parasympathetic) and somatic nervous systems (sensory and motor)[4]. Sensory information is received from the genitals towards these nervous systems, in which neurotransmitters such as serotonin, dopamine, noradrenaline, and adrenaline would be released to control erectile function[5].
Vaginal dryness refers to the situation when the vagina lacks lubrication which leads to serious pain during sexual intercourse[6]. The production of lubricants in the vagina are highly sensitive to changes in hormones such as estrogen and testosterone, that are also responsible for blood flow[7]. Low estrogen and testosterone circulating in the body contributes to vaginal dryness[7].
Sensations[edit]
Orgasms are sensory phenomena that take place in the cerebral cortex with an association with the spinal reflex[8]. Men can achieve orgasm through the penis, and can be categorised to two parts: emission and ejaculation. Neurotransmitters such as serotonin, norepinephrine and dopamine affect ejaculation in males the most[9]. For women, orgasms are induced by stimulation of erotic sites, currently there are no definitive explanations on the chemical triggers for female orgasm[10].
Types of drugs that affect sexual performance[edit]
Drugs on the market provide both benefits and detrimental effects to the person, especially regarding sexual performance, depending on the use and dosage[11]. Drugs are classified into different categories in respect to their functions, including psychoactive drugs, antihypertensive drugs, antihistamines, cancer treatment drugs and hormone medication .
Psychoactive drugs[edit]
Psychoactive drugs refer to chemical substances that affect an individual’s mental processes, such as emotions, cognition, perception, and consciousness[12]. These substances directly impact your central nervous system (CNS), which also has an impact on one’s neurophysiologic phases of sexual response[13]. Antidepressants are a group of drugs that treat individuals with clinical depression, as well as other mental disorders[14]. This group of drugs have shown to affect sexual functions in both male and females[15]. Alcohol is a group of psychoactive substances where signals of pleasure, rewards are sent to the human brain. It also causes a series of adverse effects on the body, including the brain and the liver, leading to health problems and sexual dysfunction[16][17]. Antipsychotics are drugs that treat mental disorders such as schizophrenia, and other psychoses[18]. These drugs block certain pathways in humans that contribute to sexual dysfunction, including reduced arousal and sexual desire[19].
Antihypertensive drugs[edit]
Antihypertensive drugs are a group of drugs that prevent, control and treat hypertension. Hypertension imposes negative sexual effects on both men and women, where antihypertensive drugs help alleviate erectile dysfunction in men[20].
Antihistamines[edit]
Antihistamines are used for relieving symptoms of allergies and hay fever[21]. Antihistamines may cause a drying effect of the mouth, nose and throat but can also cause a drying effect on other parts of the body, such as the vagina, decreasing moisture and lubrication[22].
Cancer treatment[edit]
There are a variety of treatment types for cancer, depending on the cancer type[23]. The therapies for treating cancer vary, including hormone therapy, medications that treat pain, depression, nerves and blood vessels. These therapies will affect one’s sexual desire and pose possible consequences on sexual response[24].
Hormone medications[edit]
Hormone therapy directs its treatment towards hormones in the body, including reproductive hormones. One type is hormonal replacement therapy (HRT), which is used to supply menopausal women that lack estrogen and progesterone, increasing vaginal lubrication[25]. Another type is testosterone replacement therapy, which treats men with hypogonadism and it helps increase libido[26]. On the contractionary, selective oestrogen receptor modulators (SERMs) lead to a drop in oestrogen levels that would cause vaginal dryness[27].
Positive Effects of Drugs on Sexual Performance[edit]
Increased libido[edit]

Libido refers to a person’s overall sexual desire and drive. Since low testosterone levels are associated with low sexual desire, testosterone replacement therapy can be prescribed for increasing testosterone in the body, increasing libido and restoring hormonal balance[28]. While Phosphodiesterase-5 (PDE5) inhibitors such as sildenafil, tadalafil, vardenafil, and avanafil are primarily known for treating erectile dysfunction, it also has a positive effect on libido[29].
Flibanserin is a drug that is both a serotonin antagonist and agonist that treats hypoactive sexual desire disorder (HSDD) for premenopausal women. The drug acts as antagonist and agonist on two different receptors. The binding of flibanserin causes downstream release of dopamine and noradrenaline and reduces the production of serotonin, increasing sex drive[30]. However, currently there is still no evidence that this drug would enhance sexual performance, therefore this drug still needs to be further investigated[30].
Increased sexual function[edit]
For males, several drugs increases the blood flow to the penis which allows for the achievement and maintenance of an erection[31]. Phosphodiesterase-5 (PDE5) inhibitors are widely known and commonly prescribed for erectile dysfunction[32]. PDE5 enzymes are blocked by PDE5 inhibitors to prevent their function, this allows for the relaxation of penile blood vessels and muscles, facilitating increased blood circulation to the penis[33]. Alprostadil injections as a vasodilator are also used for the treatment of erectile dysfunction, expanding blood vessels that result in increasing blood flow to the penis[34].
For females, vaginal lubricant production can be increased by hormone replacement therapy (HRT) medicine such as vaginal estrogen[35]. Vaginal dryness results from a declined level in circulating estrogen within the body, most likely during menopause[36]. Treatment for vaginal dryness typically involves the use of localised estrogen, such as HRT medicine. This drug works by increasing estrogen in the body circulation, thereby enhancing lubrication production in the vaginal area[36].
Achieving orgasm[edit]
Delayed ejaculation, a type of male sexual disorder that is characterised by the delay of ejaculation or inability to achieve ejaculation[37]. There are no approved drugs for the treatment of delayed ejaculation as of now, The majority of medications used for treating delayed ejaculation are primarily intended for treating different medical conditions.[38]. Amantadine, a Parkinson's medication, is known to enhance dopamine agonist release and activate dopamine receptors, which helps with ejaculation[39]. However, there is not sufficient evidence to support the effectiveness of these medications on delayed ejaculation[39].
Negative Effects of Drugs on Sexual Performance[edit]
Decreased libido[edit]
Several common medications can contribute to low libido. Antidepressants, especially selective serotonin reuptake inhibitors (SSRIs) antidepressants, increase serotonin levels that decrease testosterone, leading to a decrease in libido[40]. Antipsychotic drugs create blockages of dopamine D2 receptors that are responsible for dopamine production can lead to a low libido[19]. Additionally, these drugs can increase production of prolactin in males which contribute to lower levels of testosterone[19][41]. Chemotherapy drugs also lead to a decrease in testosterone but it is only temporary during the course of therapy[19].
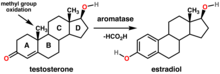
Drinking large amounts of alcohol regularly can lead to low libido due to a process called aromatisation[42]. This process refers to the conversion of testosterone or its precursors into estrogen, leading to a decrease in testosterone levels in circulation[42].
Decreased sexual function[edit]
Impotence refers to the inability of a male’s penis to become erect for sexual intercourse, in which the male is not able to get or maintain an erection[43]. The medical term for this phenomenon is erectile dysfunction. Drugs such as antihypertensives including thiazide diuretics, loop diuretics, and beta-blockers used for lowering blood pressure limiting blood flow to the penis area, making it difficult to get or maintain an erection[44]. Direct effects caused by antihypertensives on the penile vascular smooth muscle lead to vasoconstriction which leads to impaired perfusion[45]. Antipsychotic drugs are also responsible for several mechanisms that lead to erectile dysfunction. Mechanisms such as acetylcholine receptor antagonism and alpha-adrenergic receptor antagonism reduces periphery vasodilation, inducing erectile dysfunction[19].
Overindulgence in alcohol may also cause temporary inability to achieve an erection. Alcohol, being a diuretic, can cause a person to urinate more frequently, resulting in dehydration[46]. Dehydration reduces the volume of blood in the body, consequently decreasing blood flow towards the penis[46]. Additionally, dehydration also increases angiotensin levels in the body, which is a hormone associated with erectile dysfunction[46].
Birth control pills affect hormone levels in the body such as a decrease in estrogen, leading to vaginal dryness by thinning and shrinking of the vaginal tissue[7]. Moreover, SERMs such as Evista and Tamoxifen which are used to treat breast cancer, results in vaginal dryness[27].
Antihistamines narrow blood vessels, leading to lowering of moisture levels as well as mucous production, which includes lubricant production in the vagina[27]. Anti-hypertensive drugs help reduce blood pressure by decreasing blood flow to organs in the body, resulting in decreased vaginal lubrication as well[47].
Reduced sensations [edit]
Antidepressants, particularly SSRIs, cause delayed ejaculation and orgasm due to its function of retaining serotonin, which inhibits ejaculation[48]. Similarly, antipsychotics also contribute to delayed ejaculation by affecting dopamine transporters, where dopamine plays a role in ejaculation via D2 receptors[49][50].
SSRI prevents reuptake of serotonin, thereby increasing serotonin in the body and decreasing their ability to produce lubricant in the vagina. It has been reported that around 42% of women that intake this type of medication have problems with orgasm production[51]. Other medications such as antipsychotic drugs also reported signs of impaired orgasm[52].
Intake of too much alcohol can potentially cause depressant effects on the central nervous system (CNS)[53]. These effects contribute to sensory dullness, which leads to a delay effect on orgasm and ejaculation[53].
References[edit]
- ^ "Low Libido (Low Sex Drive): Causes, Symptoms & Treatment". Cleveland Clinic. Retrieved 2024-04-10.
- ^ a b "Libido - an overview | ScienceDirect Topics". www.sciencedirect.com. Retrieved 2024-04-10.
- ^ Croft, Harry A. (2017-12-14). "Understanding the Role of Serotonin in Female Hypoactive Sexual Desire Disorder and Treatment Options". The Journal of Sexual Medicine. 14 (12): 1575–1584. doi:10.1016/j.jsxm.2017.10.068.
- ^ Dean, Robert C.; Lue, Tom F. (2005). "Physiology of Penile Erection and Pathophysiology of Erectile Dysfunction". Urologic Clinics of North America. 32 (4): 379–395. doi:10.1016/j.ucl.2005.08.007. PMC 1351051. PMID 16291031.
{{cite journal}}: CS1 maint: PMC format (link) - ^ Giuliano, François; Rampin, Olivier (2004). "Neural control of erection". Physiology & Behavior. 83 (2): 189–201. doi:10.1016/j.physbeh.2004.08.014.
- ^ Bachmann, Gloria (2022). "Patient education: Vaginal dryness (Beyond the Basics)". www.uptodate.com. Retrieved 2024-04-10.
- ^ a b c "3 Medications That Can Lead To Vaginal Dryness". Health. Retrieved 2024-04-10.
- ^ "Orgasm - an overview | ScienceDirect Topics". www.sciencedirect.com. Retrieved 2024-04-10.
- ^ Melis, Maria Rosaria; Sanna, Fabrizio; Argiolas, Antonio (2022-06-24). "Dopamine, Erectile Function and Male Sexual Behavior from the Past to the Present: A Review". Brain Sciences. 12 (7): 826. doi:10.3390/brainsci12070826. ISSN 2076-3425. PMC 9312911. PMID 35884633.
{{cite journal}}: CS1 maint: PMC format (link) CS1 maint: unflagged free DOI (link) - ^ Meston, Cindy M.; Levin, Roy J.; Sipski, Marca L.; Hull, Elaine M.; Heiman, Julia R. (2004). "Women's orgasm". Annual Review of Sex Research. 15: 173–257. ISSN 1053-2528. PMID 16913280.
- ^ "Drug | Definition, Types, Interactions, Abuse, & Facts | Britannica". www.britannica.com. Retrieved 2024-04-10.
- ^ "Drugs". www.who.int. Retrieved 2024-04-10.
- ^ Galbraith, R. A. (1991). "Sexual side effects of drugs". Drug Therapy. 21 (3): 38–40, 45. ISSN 0001-7094. PMID 12316940.
- ^ "Uses - Antidepressants". nhs.uk. 2021-02-05. Retrieved 2024-04-10.
- ^ Lorenz, Tierney (2016). "Antidepressant-Induced Female Sexual Dysfunction". Mayo Clinic Proceedings.
- ^ "Alcohol's Effects on the Body | National Institute on Alcohol Abuse and Alcoholism (NIAAA)". www.niaaa.nih.gov. Retrieved 2024-04-10.
- ^ Salari, Nader; Hasheminezhad, Razie; Almasi, Afshin; Hemmati, Mahvan; Shohaimi, Shamarina; Akbari, Hakimeh; Mohammadi, Masoud (2023-05-02). "The risk of sexual dysfunction associated with alcohol consumption in women: a systematic review and meta-analysis". BMC Women's Health. 23 (1). doi:10.1186/s12905-023-02400-5. ISSN 1472-6874. PMC 10155345. PMID 37131197.
{{cite journal}}: CS1 maint: PMC format (link) CS1 maint: unflagged free DOI (link) - ^ "Oral Antipsychotic Drugs". Drug Office Department of Health. 2014.
- ^ a b c d e Park, Yeon Won; Kim, Yooseok; Lee, Jun Ho (2012). "Antipsychotic-Induced Sexual Dysfunction and Its Management". The World Journal of Men's Health. 30 (3): 153–159. doi:10.5534/wjmh.2012.30.3.153. ISSN 2287-4208. PMC 3623530. PMID 23596605.
- ^ Lou, Inmaculada Xu; Chen, Jiayue; Ali, Kamran; Chen, Qilan (2023-11-03). "Relationship Between Hypertension, Antihypertensive Drugs and Sexual Dysfunction in Men and Women: A Literature Review". Vascular Health and Risk Management. 19: 691–705. doi:10.2147/VHRM.S439334. PMC 10629452. PMID 37941540.
{{cite journal}}: CS1 maint: PMC format (link) CS1 maint: unflagged free DOI (link) - ^ "Antihistamines". nhs.uk. 2017-10-17. Retrieved 2024-04-10.
- ^ "Antihistamine (Oral Route, Parenteral Route, Rectal Route) Precautions - Mayo Clinic". www.mayoclinic.org. Retrieved 2024-04-10.
- ^ "Types of Cancer Treatment". National Cancer Institute. 2017. Retrieved 2024-04-10.
- ^ "Sexual Health Issues in Men and Cancer Treatment - Side Effects". National Cancer Institute. 2017. Retrieved 2024-04-10.
- ^ Harper-Harrison, Gina; Shanahan, Meaghan M. (2024), "Hormone Replacement Therapy", StatPearls, Treasure Island (FL): StatPearls Publishing, PMID 29630243, retrieved 2024-04-10
- ^ Osterberg, E. Charles; Bernie, Aaron M.; Ramasamy, Ranjith (2014). "Risks of testosterone replacement therapy in men". Indian Journal of Urology : IJU : Journal of the Urological Society of India. 30 (1): 2–7. doi:10.4103/0970-1591.124197. ISSN 0970-1591. PMC 3897047. PMID 24497673.
{{cite journal}}: CS1 maint: unflagged free DOI (link) - ^ a b c "Vaginal Dryness From Breast Cancer Treatment or Menopause". www.breastcancer.org. Retrieved 2024-04-10.
- ^ "Testosterone Therapy Treatment Types, Uses & Risks". Drugwatch.com. Retrieved 2024-04-10.
- ^ Korkes, Fernando; Costa-Matos, André; Gasperini, Renato; Reginato, Pedro V.; Perez, Marjo D.C. (2008-10-01). "Recreational Use of PDE5 Inhibitors by Young Healthy Men: Recognizing This Issue Among Medical Students". The Journal of Sexual Medicine. 5 (10): 2414–2418. doi:10.1111/j.1743-6109.2008.00792.x. ISSN 1743-6109.
- ^ a b Baid, Rashmi; Agarwal, Rakesh (2018). "Flibanserin: A controversial drug for female hypoactive sexual desire disorder". Industrial Psychiatry Journal. 27 (1): 154. doi:10.4103/ipj.ipj_20_16. ISSN 0972-6748. PMC 6198608. PMID 30416308.
{{cite journal}}: CS1 maint: PMC format (link) CS1 maint: unflagged free DOI (link) - ^ Steers, William D (2002). "Pharmacologic Treatment of Erectile Dysfunction". Reviews in Urology. 4 (Suppl 3): S17–S25. ISSN 1523-6161. PMC 1476024. PMID 16986010.
- ^ ElHady, Ahmed K.; El-Gamil, Dalia S.; Abdel-Halim, Mohammad; Abadi, Ashraf H. (2023). "Advancements in Phosphodiesterase 5 Inhibitors: Unveiling Present and Future Perspectives". Pharmaceuticals. 16 (9): 1266. doi:10.3390/ph16091266. ISSN 1424-8247. PMC 10536424. PMID 37765073.
{{cite journal}}: CS1 maint: PMC format (link) CS1 maint: unflagged free DOI (link) - ^ "PDE5 inhibitors: List, how they work, foods, and more". www.medicalnewstoday.com. 2020-08-17. Retrieved 2024-04-10.
- ^ "Alprostadil (Intracavernosal Route) Proper Use - Mayo Clinic". www.mayoclinic.org. Retrieved 2024-04-10.
- ^ "About vaginal oestrogen". nhs.uk. 2023-07-21. Retrieved 2024-04-10.
- ^ a b Woods, Nancy Fugate (2012). "An overview of chronic vaginal atrophy and options for symptom management". Nursing for Women's Health. 16 (6): 482–493, quiz 494. doi:10.1111/j.1751-486X.2012.01776.x. ISSN 1751-486X. PMID 23253575.
- ^ Abdel-Hamid, Ibrahim A.; Ali, Omar I. (2018). "Delayed Ejaculation: Pathophysiology, Diagnosis, and Treatment". The World Journal of Men's Health. 36 (1): 22–40. doi:10.5534/wjmh.17051. ISSN 2287-4208. PMC 5756804. PMID 29299903.
- ^ Print, Mayo Clinic Staff. "Delayed ejaculation - Treatment". Mayo Clinic. Retrieved 2024-04-10.
- ^ a b Abdel-Hamid, Ibrahim A.; Elsaied, Moustafa A.; Mostafa, Taymour (2016). "The drug treatment of delayed ejaculation". Translational Andrology and Urology. 5 (4): 576–591. doi:10.21037/tau.2016.05.05. ISSN 2223-4691. PMC 5001980. PMID 27652229.
{{cite journal}}: CS1 maint: unflagged free DOI (link) - ^ Jing, Elizabeth; Straw-Wilson, Kristyn (2016-06-29). "Sexual dysfunction in selective serotonin reuptake inhibitors (SSRIs) and potential solutions: A narrative literature review". The Mental Health Clinician. 6 (4): 191–196. doi:10.9740/mhc.2016.07.191. ISSN 2168-9709. PMC 6007725. PMID 29955469.
- ^ J Snyder, Peter. "Patient education: High prolactin levels and prolactinomas (Beyond the Basics)". UpToDate. Retrieved 2024-04-10.
- ^ a b Emanuele, M. A.; Emanuele, N. V. (1998). "Alcohol's effects on male reproduction". Alcohol Health and Research World. 22 (3): 195–201. ISSN 0090-838X. PMC 6761906. PMID 15706796.
- ^ "Impotence (Erectile Dysfunction)". Harvard Health. 2018-12-11. Retrieved 2024-04-10.
- ^ "Blood pressure drugs and ED: What you need to know". Harvard Health. 2017-05-30. Retrieved 2024-04-10.
- ^ Chrysant, Steven G. (2015). "Antihypertensive therapy causes erectile dysfunction". Current Opinion in Cardiology. 30 (4): 383–390. doi:10.1097/HCO.0000000000000189. ISSN 0268-4705.
- ^ a b c Baxter, Rachel. "Alcohol and Temporary Erectile Dysfunction". SMSNA. Retrieved 2024-04-10.
- ^ Neel, Armon B. (2012). "7 Meds That Can Wreck Your Sex Life". AARP.
- ^ Giuliano, François; Clément, Pierre (2006). "Serotonin and Premature Ejaculation: From Physiology to Patient Management". European Urology. 50 (3): 454–466. doi:10.1016/j.eururo.2006.05.055.
- ^ Kalejaiye, Odunayo; Almekaty, Khaled; Blecher, Gideon; Minhas, Suks (2017-12-04). "Premature ejaculation: challenging new and the old concepts". F1000Research. 6: 2084. doi:10.12688/f1000research.12150.1. ISSN 2046-1402. PMC 5717471. PMID 29259775.
{{cite journal}}: CS1 maint: PMC format (link) CS1 maint: unflagged free DOI (link) - ^ Gur, S.; Sikka, S. C. (2015). "The characterization, current medications, and promising therapeutics targets for premature ejaculation". Andrology. 3 (3): 424–442. doi:10.1111/andr.12032.
- ^ Lorenz, Tierney; Rullo, Jordan; Faubion (2016). "Antidepressant-Induced Female Sexual Dysfunction". Mayo Clinic Proceedings. 91 (9): 1280–1286. doi:10.1016/j.mayocp.2016.04.033. PMC 6711470. PMID 27594188.
{{cite journal}}: CS1 maint: PMC format (link) - ^ Just, Marek Jan (2015). "The influence of atypical antipsychotic drugs on sexual function". Neuropsychiatric Disease and Treatment: 1655. doi:10.2147/NDT.S84528. ISSN 1178-2021.
{{cite journal}}: CS1 maint: unflagged free DOI (link) - ^ a b "Alcohol & Male Libido: The Effects | Manual". www.manual.co. Retrieved 2024-04-10.
